Sunday Poster Session
Category: Interventional Endoscopy
P1075 - Pancreatic Tail Cyst Causing Hydronephrosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Andrej M. Sodoma, DO
South Shore University Hospital
Selden, NY
Presenting Author(s)
Andrej Sodoma, DO1, James R. Pellegrini, MD2, Nicholas Bulba, BA3, Jaspreet Singh, MD4
1South Shore University Hospital, Bay Shore, NY; 2Nassau University Medical Center, Great River, NY; 3NYIT College of Osteopathic Medicine, Brooklyn, NY; 4Northwell Health, Bayshore, NY
Introduction: Pancreatic cysts are either cancerous or benign. Most people with them are asymptomatic, so they are usually found incidentally on imaging. At times, these cysts can become so large that they obstruct the function of structures around them, causing jaundice or pancreatitis. In this case, a pancreatic pseudocyst became so large that it caused hydronephrosis.
Case Description/Methods: 95-year-old Female with a past medical history of HFpEF, sick sinus syndrome with a pacemaker, chronic afib, history of DVT on Pradaxa, hypothyroid, sleep apnea, history of vertebral fixation with kyphoplasty presented to a tertiary care university hospital center with abdominal pain. CT on that admission noted intraductal papillary mucinous neoplasm with ductal dilatation worrisome for underlying malignancy. GI was consulted, and an MRI was recommended; however, the patient's pacemaker was not MRI-compatible. The patient’s abdominal pain improved, and so she was discharged for outpatient EUS. The patient then experienced RUQ pain, nausea, and decreased oral intake. CT on return to the hospital showed a new pancreatic pseudocyst causing left hydronephrosis, which was not present on the prior exam. The patient then went for EGD and EUS with cyst gastrostomy drainage. An extensive peri-pancreatic fluid collection was identified, measuring approximately 11cm X 7cm. A 15mm Hot Axios (LAMS) cyst gastrostomy tube was placed, cytopathology report was negative for malignant cells. Repeat CT abdomen post-procedure showed the Axios drain in place with near complete resolution of pseudocyst at the pancreatic tail with stable severe dilatation of pancreatic duct. A repeat EGD was performed, showing the complete resolution of the prior pseudocyst. The cyst gastrostomy LAMS tube was removed and confirmed intact. The patient tolerated a diet shortly after the procedure, with no complaints, abdominal tenderness, afebrile, or leukocytosis. The patient was discharged home with close follow-up with GI.
Discussion: The pancreatic cyst was drained, and the fluid sent for cytology was found to be non-malignant. The prognosis of pancreatic cysts depends on the cyst's contents. Pancreatic pseudocysts sometimes resolve in 2-6 weeks; if they do not, they require surgery or endoscopy. Advancements in surgery have made cystogastrostomy and cystojejunostomy tubes solutions to the issue with a great success rate.

Disclosures:
Andrej Sodoma, DO1, James R. Pellegrini, MD2, Nicholas Bulba, BA3, Jaspreet Singh, MD4. P1075 - Pancreatic Tail Cyst Causing Hydronephrosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1South Shore University Hospital, Bay Shore, NY; 2Nassau University Medical Center, Great River, NY; 3NYIT College of Osteopathic Medicine, Brooklyn, NY; 4Northwell Health, Bayshore, NY
Introduction: Pancreatic cysts are either cancerous or benign. Most people with them are asymptomatic, so they are usually found incidentally on imaging. At times, these cysts can become so large that they obstruct the function of structures around them, causing jaundice or pancreatitis. In this case, a pancreatic pseudocyst became so large that it caused hydronephrosis.
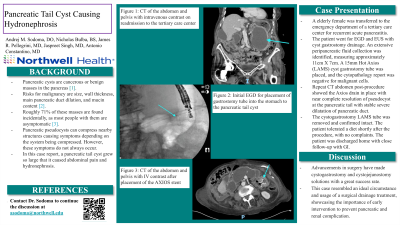
Case Description/Methods: 95-year-old Female with a past medical history of HFpEF, sick sinus syndrome with a pacemaker, chronic afib, history of DVT on Pradaxa, hypothyroid, sleep apnea, history of vertebral fixation with kyphoplasty presented to a tertiary care university hospital center with abdominal pain. CT on that admission noted intraductal papillary mucinous neoplasm with ductal dilatation worrisome for underlying malignancy. GI was consulted, and an MRI was recommended; however, the patient's pacemaker was not MRI-compatible. The patient’s abdominal pain improved, and so she was discharged for outpatient EUS. The patient then experienced RUQ pain, nausea, and decreased oral intake. CT on return to the hospital showed a new pancreatic pseudocyst causing left hydronephrosis, which was not present on the prior exam. The patient then went for EGD and EUS with cyst gastrostomy drainage. An extensive peri-pancreatic fluid collection was identified, measuring approximately 11cm X 7cm. A 15mm Hot Axios (LAMS) cyst gastrostomy tube was placed, cytopathology report was negative for malignant cells. Repeat CT abdomen post-procedure showed the Axios drain in place with near complete resolution of pseudocyst at the pancreatic tail with stable severe dilatation of pancreatic duct. A repeat EGD was performed, showing the complete resolution of the prior pseudocyst. The cyst gastrostomy LAMS tube was removed and confirmed intact. The patient tolerated a diet shortly after the procedure, with no complaints, abdominal tenderness, afebrile, or leukocytosis. The patient was discharged home with close follow-up with GI.
Discussion: The pancreatic cyst was drained, and the fluid sent for cytology was found to be non-malignant. The prognosis of pancreatic cysts depends on the cyst's contents. Pancreatic pseudocysts sometimes resolve in 2-6 weeks; if they do not, they require surgery or endoscopy. Advancements in surgery have made cystogastrostomy and cystojejunostomy tubes solutions to the issue with a great success rate.

Figure: CT abdomen and pelvis with IV contrast post-drainage of pancreatic cyst.
Disclosures:
Andrej Sodoma indicated no relevant financial relationships.
James Pellegrini indicated no relevant financial relationships.
Nicholas Bulba indicated no relevant financial relationships.
Jaspreet Singh indicated no relevant financial relationships.
Andrej Sodoma, DO1, James R. Pellegrini, MD2, Nicholas Bulba, BA3, Jaspreet Singh, MD4. P1075 - Pancreatic Tail Cyst Causing Hydronephrosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
