Sunday Poster Session
Category: Interventional Endoscopy
P1079 - Esophageal Perforation After Percutaneous Endoscopic Gastrostomy (PEG) Tube Placement: A Complication Treated Successfully With Endoscopic Stent and Suture
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Asad Rehman, DO
HCA Kingwood
San Antonio, TX
Presenting Author(s)
Asad Rehman, DO1, Suhail Kayyali, DO2, Bobby Jacob, MD2, Ammar Hasan, MD1, Bushra Bangash, MD1, Mahnoor Hashmi, MD1, Meir Mizrahi, MD3, Ismail Hader, MD1
1HCA Kingwood, Kingwood, TX; 2HCA Healthcare, Largo, FL; 3HCA Florida Largo Hospital, Largo, FL
Introduction: Surgical repair has been the standard approach for esophageal perforation; however, there is growing evidence supporting the role of endoscopic stenting depending on the size and location of the defect. This case showcases endoscopic suturing for the treatment of an esophageal perforation due to percutaneous endoscopic gastrostomy (PEG) tube placement.
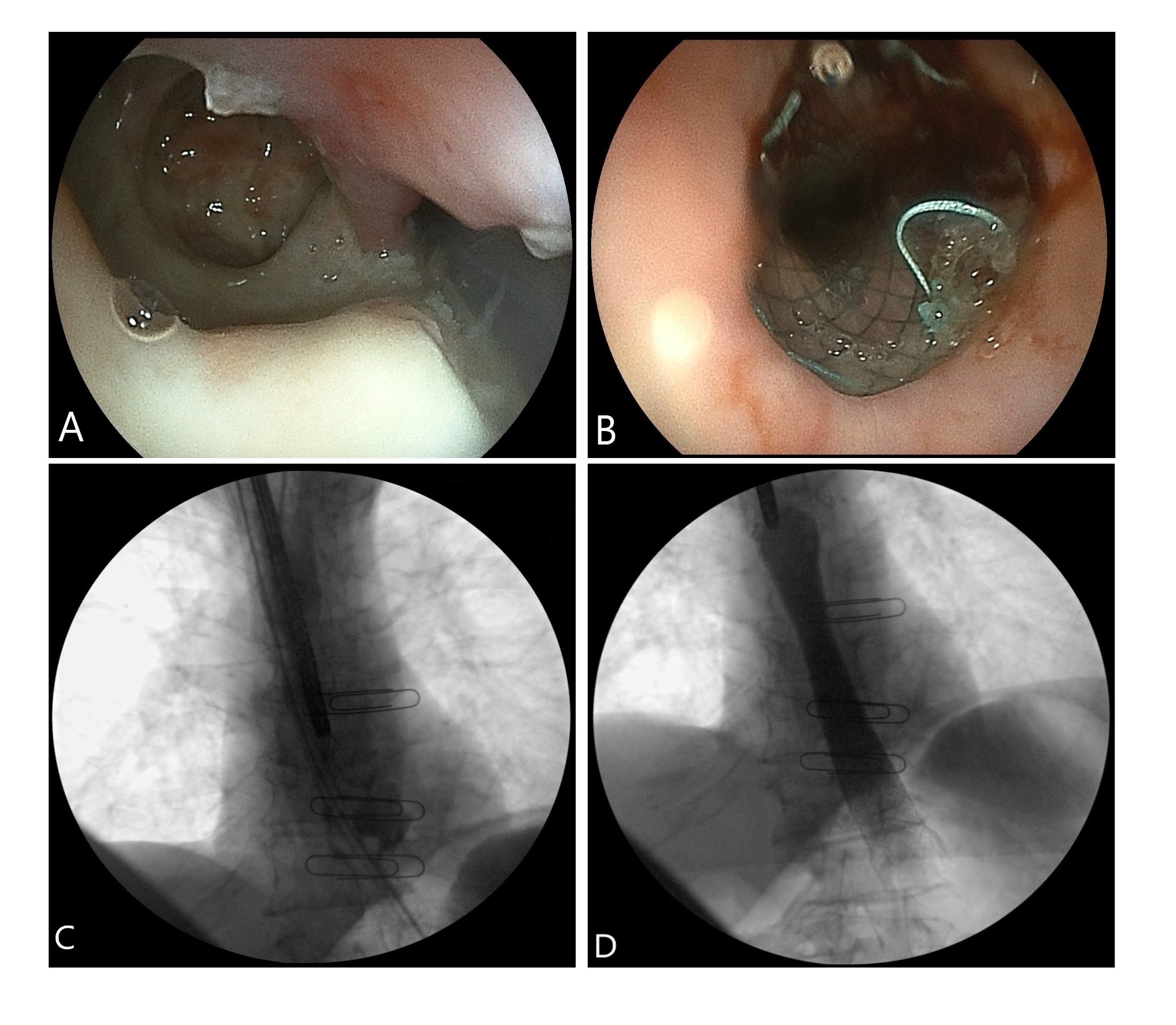
Case Description/Methods: A 69-year-old female with malignant distal esophageal stricture secondary to stage II squamous cell carcinoma presented as a transfer for esophageal perforation after planned esophageal dilation and PEG tube placement. The stricture was dilated with wire-guided balloon for PEG tube placement. After pulling the PEG tube, a nonbleeding mucosal defect in the distal esophagus proximal to the gastroesophageal junction was noted. A nasogastric (NG) tube was placed proximally, and the remaining gastric tube was placed. Computed tomography (CT) scan of the chest with contrast showed a mediastinal air posterior to the esophagus. During esophagogastroduodenoscopy (EGD), the full-thickness posterior esophageal wall defect was noted at 32 cm to 37 cm from the incisors. A fully covered esophageal stent was placed over the wire across the defect and endoscopically sutured. Contrast was injected and the esophagogram confirmed no further extravasation. The patient was treated with intravenous pantoprazole and antibiotics. Chest x-ray showed no stent migration. The patient was transitioned to a clear liquid diet without any pain.
Discussion: Esophageal perforation is a potentially fatal complication of endoscopic procedures. Early detection and appropriate treatment are essential to prevent fatal outcomes. Surgical closure of esophageal perforations remains the standard treatment, despite morbidity and mortality rates of up to 36% and 10%, respectively. Studies have shown endoscopic closure with stents to completely heal mucosal defects in over 85% of cases. Despite being technically more challenging than clip placement, the versatility of endoscopic sutures offers closures of acute perforations and chronic fistulas. Patients with esophageal perforations treated nonoperatively have shorter hospital stays (13 vs 24 days), fewer complications (36% vs 62%), and less mortality (4% vs 15%) than those managed operatively. Endoscopic suturing is an innovative technique that shows promise for treating esophageal perforation in acute settings to decrease both morbidity and mortality. As a result, endoscopic closure can be considered over surgery.
Disclosures:
Asad Rehman, DO1, Suhail Kayyali, DO2, Bobby Jacob, MD2, Ammar Hasan, MD1, Bushra Bangash, MD1, Mahnoor Hashmi, MD1, Meir Mizrahi, MD3, Ismail Hader, MD1. P1079 - Esophageal Perforation After Percutaneous Endoscopic Gastrostomy (PEG) Tube Placement: A Complication Treated Successfully With Endoscopic Stent and Suture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Kingwood, Kingwood, TX; 2HCA Healthcare, Largo, FL; 3HCA Florida Largo Hospital, Largo, FL
Introduction: Surgical repair has been the standard approach for esophageal perforation; however, there is growing evidence supporting the role of endoscopic stenting depending on the size and location of the defect. This case showcases endoscopic suturing for the treatment of an esophageal perforation due to percutaneous endoscopic gastrostomy (PEG) tube placement.
Case Description/Methods: A 69-year-old female with malignant distal esophageal stricture secondary to stage II squamous cell carcinoma presented as a transfer for esophageal perforation after planned esophageal dilation and PEG tube placement. The stricture was dilated with wire-guided balloon for PEG tube placement. After pulling the PEG tube, a nonbleeding mucosal defect in the distal esophagus proximal to the gastroesophageal junction was noted. A nasogastric (NG) tube was placed proximally, and the remaining gastric tube was placed. Computed tomography (CT) scan of the chest with contrast showed a mediastinal air posterior to the esophagus. During esophagogastroduodenoscopy (EGD), the full-thickness posterior esophageal wall defect was noted at 32 cm to 37 cm from the incisors. A fully covered esophageal stent was placed over the wire across the defect and endoscopically sutured. Contrast was injected and the esophagogram confirmed no further extravasation. The patient was treated with intravenous pantoprazole and antibiotics. Chest x-ray showed no stent migration. The patient was transitioned to a clear liquid diet without any pain.
Discussion: Esophageal perforation is a potentially fatal complication of endoscopic procedures. Early detection and appropriate treatment are essential to prevent fatal outcomes. Surgical closure of esophageal perforations remains the standard treatment, despite morbidity and mortality rates of up to 36% and 10%, respectively. Studies have shown endoscopic closure with stents to completely heal mucosal defects in over 85% of cases. Despite being technically more challenging than clip placement, the versatility of endoscopic sutures offers closures of acute perforations and chronic fistulas. Patients with esophageal perforations treated nonoperatively have shorter hospital stays (13 vs 24 days), fewer complications (36% vs 62%), and less mortality (4% vs 15%) than those managed operatively. Endoscopic suturing is an innovative technique that shows promise for treating esophageal perforation in acute settings to decrease both morbidity and mortality. As a result, endoscopic closure can be considered over surgery.
Figure: A) 5 cm full thickness posterior esophageal wall defect noted starting at 32cm from the incisors before intervention. B) 23 mm x 125 mm fully covered esophageal stent placed over the defect and endoscopically sutured with one suture to prevent stent migration. C) Endoscopic contrast injection was performed under fluoroscopic imaging which confirmed esophageal perforation and leak prior to intervention. D) Contrast was subsequently injected endoscopically after intervention which confirmed no further extravasation of contrast.
Disclosures:
Asad Rehman indicated no relevant financial relationships.
Suhail Kayyali indicated no relevant financial relationships.
Bobby Jacob indicated no relevant financial relationships.
Ammar Hasan indicated no relevant financial relationships.
Bushra Bangash indicated no relevant financial relationships.
Mahnoor Hashmi indicated no relevant financial relationships.
Meir Mizrahi indicated no relevant financial relationships.
Ismail Hader indicated no relevant financial relationships.
Asad Rehman, DO1, Suhail Kayyali, DO2, Bobby Jacob, MD2, Ammar Hasan, MD1, Bushra Bangash, MD1, Mahnoor Hashmi, MD1, Meir Mizrahi, MD3, Ismail Hader, MD1. P1079 - Esophageal Perforation After Percutaneous Endoscopic Gastrostomy (PEG) Tube Placement: A Complication Treated Successfully With Endoscopic Stent and Suture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
