Sunday Poster Session
Category: IBD
P0989 - Acute severe ulcerative colitis with major acute gastrointestinal hemorrhage
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Malik Mushannen, MD
New York-Presbyterian / Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Malik Mushannen, MD1, Alan Zakko, MD2, Anas Zaher, MD1, Megha Kothari, MD3
1New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian Brooklyn Methodist Hospital, New York, NY; 3New York Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Rectal bleeding is common in patients with inflammatory bowel disease (1). However, major acute gastrointestinal hemorrhage is a rarer manifestation. We present a case of large volume hematochezia from a visible colonic vessel in the setting of medically refractory acute ulcerative colitis.
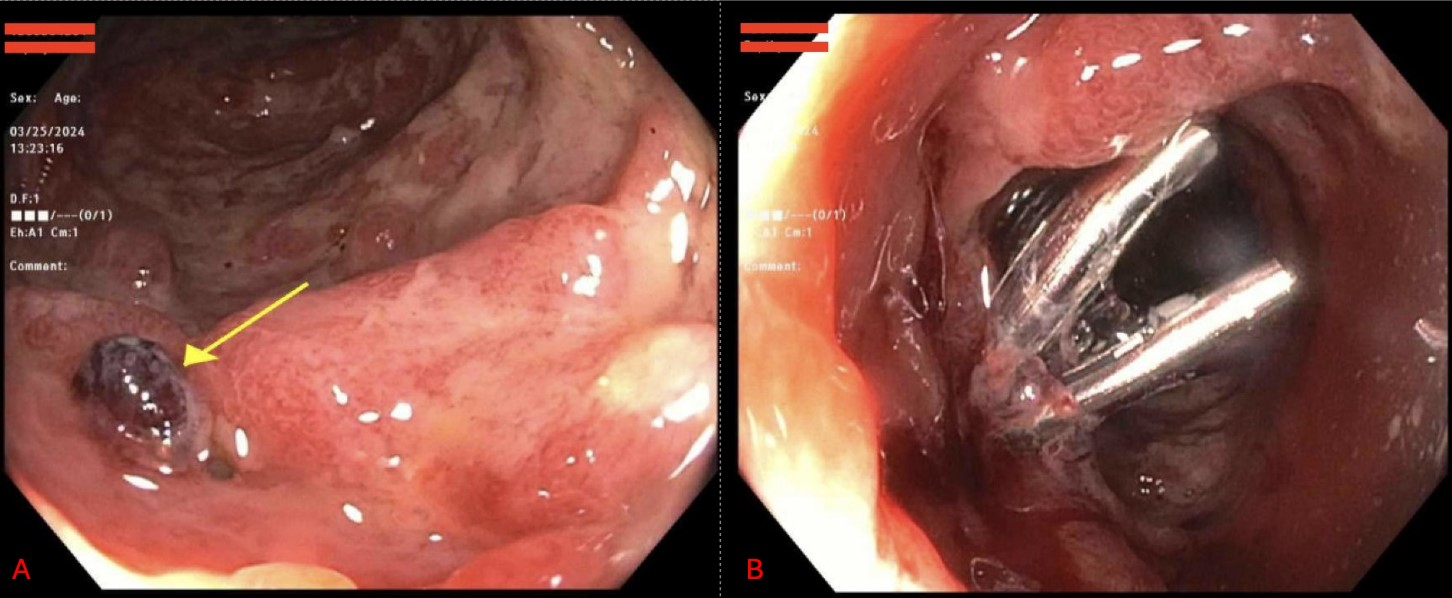
Case Description/Methods: A 55-year-old man with a past medical history of ulcerative colitis presented to the emergency department with 4 months of abdominal pain and bloody diarrhea. On admission, the patient’s vital signs were stable. His labs showed a leukocytosis with 20% bands, hemoglobin of 9.6 g/dL, and CRP of 161 mg/L. Computed tomography of his abdomen and pelvis revealed bowel wall thickening consistent with colitis. Stool studies revealed no infection and fecal calprotectin was >3000 ug/g. A flexible sigmoidoscopy revealed Mayo score 3 colitis contiguous from the rectum to the descending colon. He was diagnosed with acute severe ulcerative colitis. Methylprednisolone 60 mg daily was given for 3 days with only minimal improvement in inflammatory markers and symptoms. Given failure to steroids, the patient was started on infliximab 10 mg/kg. He then experienced large volume hematochezia with a concomitant hemoglobin drop. He received packed red blood cell transfusions for a hemoglobin under 7 g/dL. An urgent flexible sigmoidoscopy revealed a visible vessel with adherent clot in the sigmoid colon. This was treated with two hemostatic clips (figure A and B). He had no further episodes of large volume hematochezia. However, given signs of medically refractory acute ulcerative colitis, a colectomy was recommended. Instead, the patient opted to leave against medical advice from our hospital with a plan to drive to another state to undergo surgery.
Discussion: Acute gastrointestinal hemorrhage is uncommon in inflammatory bowel disease. Most cases are due to Crohn’s disease with deep ulceration. In one study, 0.1% of patients presenting with ulcerative colitis had major acute bleeding while 1.2% of patients with Crohn’s disease had major bleeding (1). While surgery is required in some instances of severe bleeding, our case demonstrated the importance of early endoscopic evaluation as it led to finding a targetable lesion for hemostatic intervention.
Disclosures:
Malik Mushannen, MD1, Alan Zakko, MD2, Anas Zaher, MD1, Megha Kothari, MD3. P0989 - Acute severe ulcerative colitis with major acute gastrointestinal hemorrhage, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian Brooklyn Methodist Hospital, New York, NY; 3New York Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Rectal bleeding is common in patients with inflammatory bowel disease (1). However, major acute gastrointestinal hemorrhage is a rarer manifestation. We present a case of large volume hematochezia from a visible colonic vessel in the setting of medically refractory acute ulcerative colitis.
Case Description/Methods: A 55-year-old man with a past medical history of ulcerative colitis presented to the emergency department with 4 months of abdominal pain and bloody diarrhea. On admission, the patient’s vital signs were stable. His labs showed a leukocytosis with 20% bands, hemoglobin of 9.6 g/dL, and CRP of 161 mg/L. Computed tomography of his abdomen and pelvis revealed bowel wall thickening consistent with colitis. Stool studies revealed no infection and fecal calprotectin was >3000 ug/g. A flexible sigmoidoscopy revealed Mayo score 3 colitis contiguous from the rectum to the descending colon. He was diagnosed with acute severe ulcerative colitis. Methylprednisolone 60 mg daily was given for 3 days with only minimal improvement in inflammatory markers and symptoms. Given failure to steroids, the patient was started on infliximab 10 mg/kg. He then experienced large volume hematochezia with a concomitant hemoglobin drop. He received packed red blood cell transfusions for a hemoglobin under 7 g/dL. An urgent flexible sigmoidoscopy revealed a visible vessel with adherent clot in the sigmoid colon. This was treated with two hemostatic clips (figure A and B). He had no further episodes of large volume hematochezia. However, given signs of medically refractory acute ulcerative colitis, a colectomy was recommended. Instead, the patient opted to leave against medical advice from our hospital with a plan to drive to another state to undergo surgery.
Discussion: Acute gastrointestinal hemorrhage is uncommon in inflammatory bowel disease. Most cases are due to Crohn’s disease with deep ulceration. In one study, 0.1% of patients presenting with ulcerative colitis had major acute bleeding while 1.2% of patients with Crohn’s disease had major bleeding (1). While surgery is required in some instances of severe bleeding, our case demonstrated the importance of early endoscopic evaluation as it led to finding a targetable lesion for hemostatic intervention.
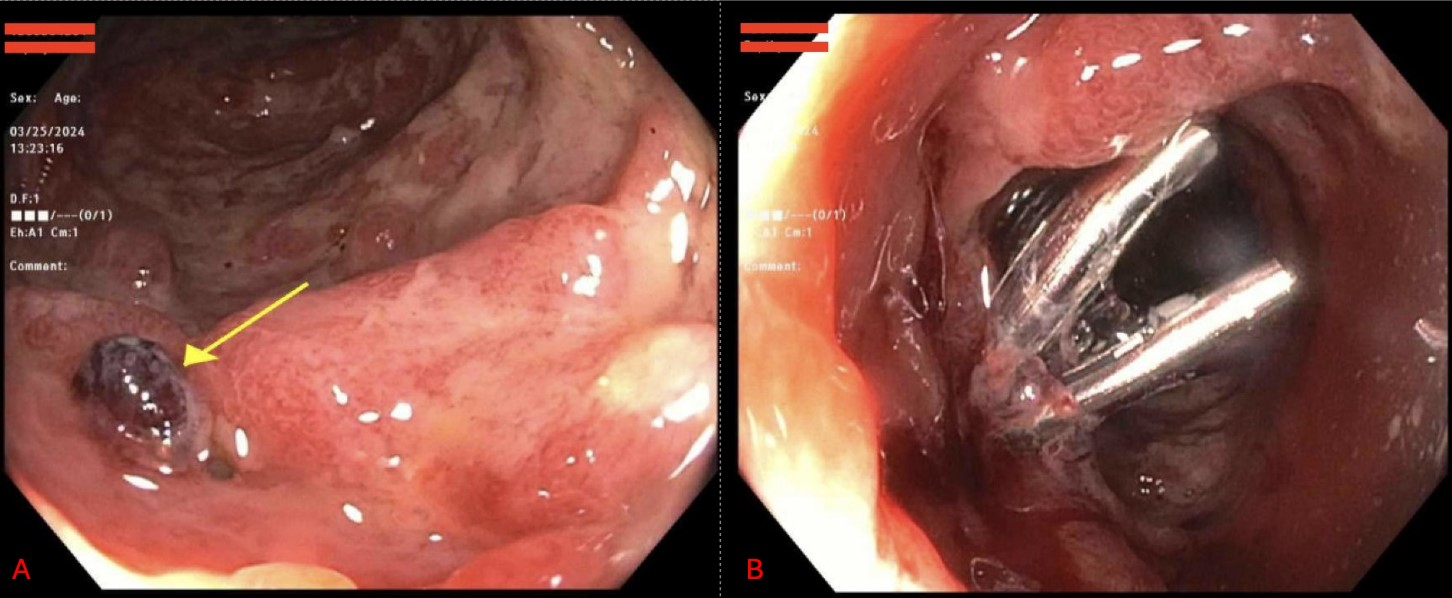
Figure: Figure A: Visible vessel seen in the sigmoid colon
Figure B: Visible vessel in sigmoid colon after placement of 2 hemostatic clips
Figure B: Visible vessel in sigmoid colon after placement of 2 hemostatic clips
Disclosures:
Malik Mushannen indicated no relevant financial relationships.
Alan Zakko indicated no relevant financial relationships.
Anas Zaher indicated no relevant financial relationships.
Megha Kothari indicated no relevant financial relationships.
Malik Mushannen, MD1, Alan Zakko, MD2, Anas Zaher, MD1, Megha Kothari, MD3. P0989 - Acute severe ulcerative colitis with major acute gastrointestinal hemorrhage, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
