Sunday Poster Session
Category: IBD
P0991 - A Sneaky Leak: Idiopathic Spontaneous Pneumomediastinum in an Active Crohn’s Patient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Jake Cresta, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Jake Cresta, MD, Azfar S. Syed, DO, MBA, Jared Magee, DO, MPH, John G.. McCarthy, MD
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: The development of spontaneous pneumomediastinum (SPM) is most commonly due to esophageal perforations. When rarely associated with inflammatory bowel disease (IBD), SPM is typically linked to colonic perforation, toxic megacolon, or preceding endoscopic procedures. Here we describe a case of Crohn’s disease (CD) complicated by idiopathic SPM in the setting of prolonged corticosteroid use.
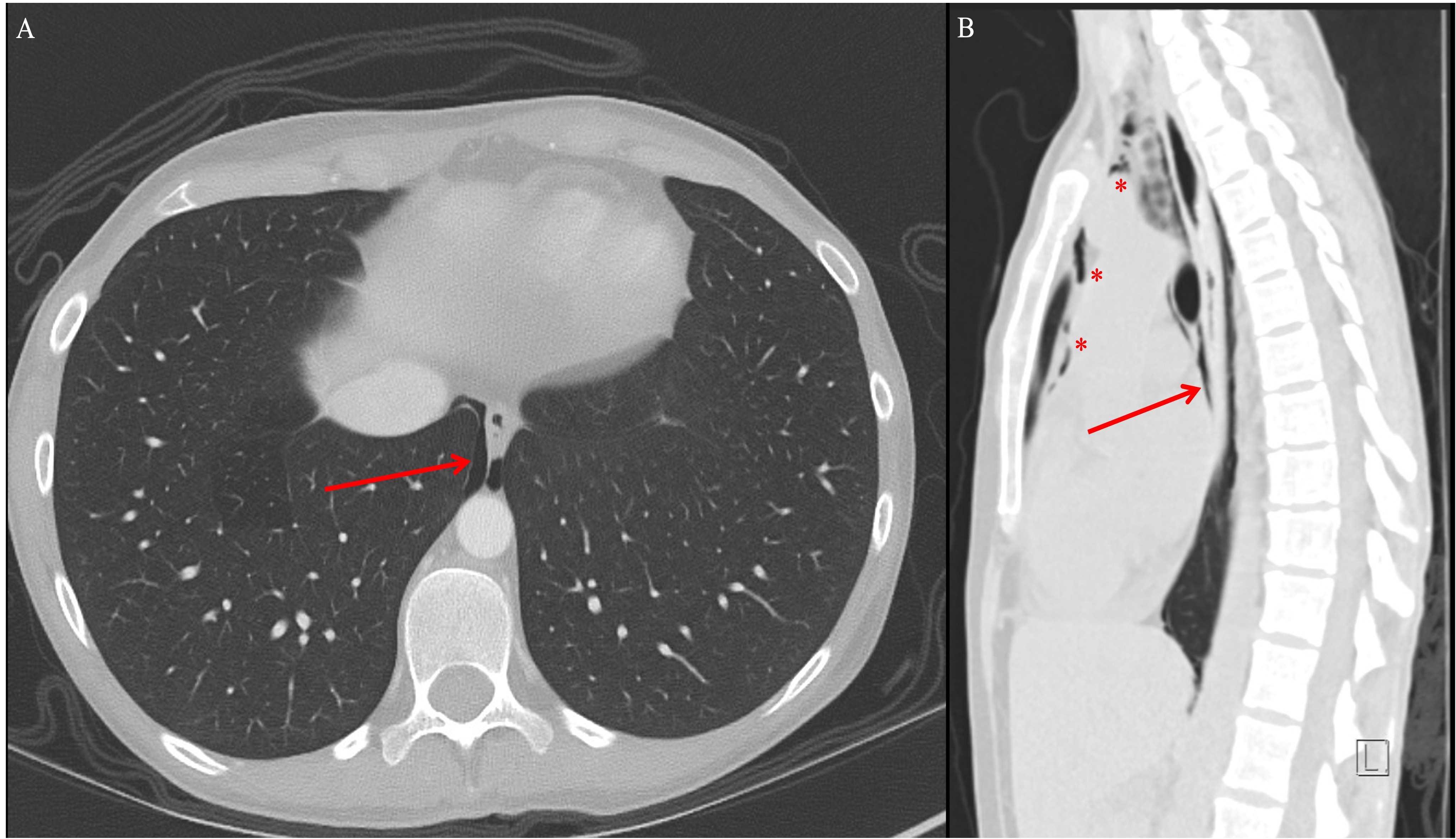
Case Description/Methods: A 30-year-old active-duty female nonsmoker with a history of ileocolonic CD with peri-anal modifiers was hospitalized due to weeks of increasing lower abdominal pain and stool changes indicative of an acute IBD flare. She reported nocturnal bowel movements, fecal urgency, and occasional pyrosis relieved by famotidine. She denied respiratory complaints, dysphagia, emesis, or recent esophageal or colonic procedures. Her disease had been difficult to control, and she had failed anti-tumor necrosis factor therapy previously. At presentation, she had been on prednisone for 6 weeks and was pending her last vedolizumab induction dose. She had stable vitals and pulmonary exam findings. Mild lower abdominal tenderness was noted without peritoneal signs. Laboratory tests revealed leukocytosis, thrombocytosis, elevated CRP and ESR levels. Computed Tomography (CT) scans showed diffuse thickening and enhancement of the colon and incidental pneumomediastinum with contained air around the lower esophagus (Figure 1). A gastrografin esophagram followed by a CT chest scan with oral contrast ruled out esophageal perforation. Her SPM was treated in conjunction with thoracic surgery conservatively with amoxicillin-clavulanic acid, and fluconazole for a total of 7 days. She received IV methylprednisone for her CD flare which was able to capture her disease and she received her last induction vedolizumab dose prior to discharge home.
Discussion: Isolated SPM in IBD is rare and usually happens in the setting of active inflammation resulting in transient bowel microperforations. Our patient, was on chronic stress dose steroids for 6 weeks preceding her presentation, with sub-optimal control of her CD. We postulate that chronic steroid-induced immunosuppression weakened her esophageal tissue, leading to SPM. Similar cases have noted this vulnerability in patients with autoimmune conditions on long-term steroids. This case highlights a rare, potentially serious consequence of chronic steroid use in an IBD patient, which further reinforces the importance of controlling IBD with steroid sparing agents.
Disclosures:
Jake Cresta, MD, Azfar S. Syed, DO, MBA, Jared Magee, DO, MPH, John G.. McCarthy, MD. P0991 - A Sneaky Leak: Idiopathic Spontaneous Pneumomediastinum in an Active Crohn’s Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: The development of spontaneous pneumomediastinum (SPM) is most commonly due to esophageal perforations. When rarely associated with inflammatory bowel disease (IBD), SPM is typically linked to colonic perforation, toxic megacolon, or preceding endoscopic procedures. Here we describe a case of Crohn’s disease (CD) complicated by idiopathic SPM in the setting of prolonged corticosteroid use.
Case Description/Methods: A 30-year-old active-duty female nonsmoker with a history of ileocolonic CD with peri-anal modifiers was hospitalized due to weeks of increasing lower abdominal pain and stool changes indicative of an acute IBD flare. She reported nocturnal bowel movements, fecal urgency, and occasional pyrosis relieved by famotidine. She denied respiratory complaints, dysphagia, emesis, or recent esophageal or colonic procedures. Her disease had been difficult to control, and she had failed anti-tumor necrosis factor therapy previously. At presentation, she had been on prednisone for 6 weeks and was pending her last vedolizumab induction dose. She had stable vitals and pulmonary exam findings. Mild lower abdominal tenderness was noted without peritoneal signs. Laboratory tests revealed leukocytosis, thrombocytosis, elevated CRP and ESR levels. Computed Tomography (CT) scans showed diffuse thickening and enhancement of the colon and incidental pneumomediastinum with contained air around the lower esophagus (Figure 1). A gastrografin esophagram followed by a CT chest scan with oral contrast ruled out esophageal perforation. Her SPM was treated in conjunction with thoracic surgery conservatively with amoxicillin-clavulanic acid, and fluconazole for a total of 7 days. She received IV methylprednisone for her CD flare which was able to capture her disease and she received her last induction vedolizumab dose prior to discharge home.
Discussion: Isolated SPM in IBD is rare and usually happens in the setting of active inflammation resulting in transient bowel microperforations. Our patient, was on chronic stress dose steroids for 6 weeks preceding her presentation, with sub-optimal control of her CD. We postulate that chronic steroid-induced immunosuppression weakened her esophageal tissue, leading to SPM. Similar cases have noted this vulnerability in patients with autoimmune conditions on long-term steroids. This case highlights a rare, potentially serious consequence of chronic steroid use in an IBD patient, which further reinforces the importance of controlling IBD with steroid sparing agents.
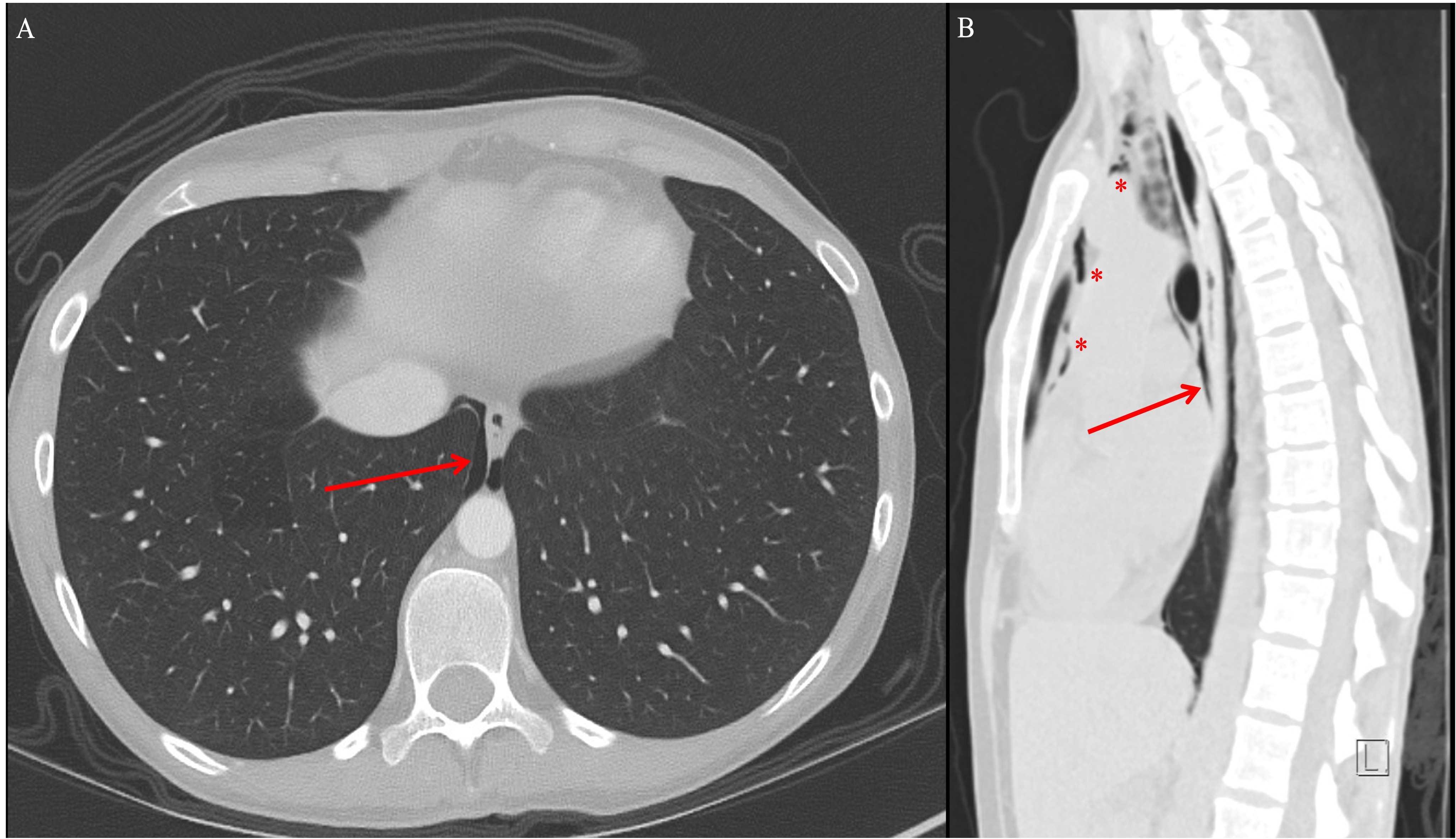
Figure: Figure 1 - CT of the Chest: Axial (Panel A) and sagittal (Panel B) images obtained without the administration of oral or intravenous contrast material show nonspecific pneumomediastinum with contained air seen surrounding the lower esophagus (Panels A and B, arrows). Free air is also seen extending along the anterior and superior mediastinum (Panel B, asterisks).
Disclosures:
Jake Cresta indicated no relevant financial relationships.
Azfar Syed indicated no relevant financial relationships.
Jared Magee indicated no relevant financial relationships.
John McCarthy indicated no relevant financial relationships.
Jake Cresta, MD, Azfar S. Syed, DO, MBA, Jared Magee, DO, MPH, John G.. McCarthy, MD. P0991 - A Sneaky Leak: Idiopathic Spontaneous Pneumomediastinum in an Active Crohn’s Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
