Sunday Poster Session
Category: IBD
P0997 - "Orange" You Glad It Wasn’t Jaundice? Carotenemia due to Dietary Modifications to Manage Crohn’s Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Erin L. Currey, MD
Wright Patterson Medical Center
Wright-Patterson AFB, OH
Presenting Author(s)
Erin L. Currey, MD1, Michael Brazeau, DO1, Christopher Casaccio, DO2
1Wright Patterson Medical Center, Wright-Patterson AFB, OH; 2Wright-Patterson Medical Center, Wright-Patterson AFB, OH
Introduction: This case report highlights a patient with Crohn’s disease (CD) who was initially lost to follow-up due to self-management of symptoms with high dietary fiber intake, who’s second presentation to care was to the emergency department with painless “jaundice” ultimately found to be hypercarotenemia from excessive carrot intake.
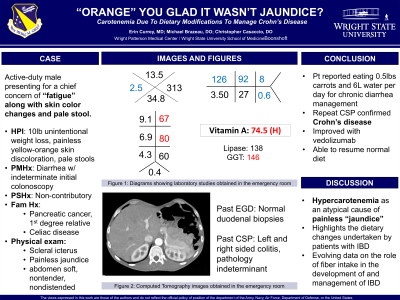
Case Description/Methods: Patient is an active-duty male with a family history of pancreatic cancer and celiac disease who presented to the ER for fatigue, 10lbs of unintentional weight loss over three months, dark stools without blood, and painless “jaundice.” Labs were remarkable for leukopenia, macrocytic anemia, AST 67, ALT 80, GGT 146, and normal total and direct bilirubin. CT abdomen and pelvis was without acute intrabdominal process. With additional history, it was found that patient was consuming a minimum of half a pound of carrots daily to control his long-standing diarrhea and abdominal pain, leading to a presumptive diagnosis of hypercarotinemia. Vitamin A level was 74.5 ug/dL (H). Of note, patient had previously been evaluated for colitis approximately five years prior. Initial colonoscopy was suspicious but not diagnostic for Crohn’s disease, and the patient was instructed to return for repeat colonoscopy to document chronicity. However, he was lost to follow up for several years and self-titrated his dietary fiber intake to improve his symptoms. Patient now has substantially improved on vedolizumab and skin discoloration improved with reduction in carrot intake.
Discussion: This case highlights an atypical cause of painless “jaundice” and the substantial dietary modifications that patients with IBD often take to manage their abdominal symptoms. Several studies including a Cochrane review and a systematic review in Nutrients have looked into the role of dietary fiber in both the pathogenesis and management of IBD. However, findings from both were limited by inclusion of multiple subtypes of IBD, inadequate power, and high risk for bias. However, epidemiologic studies have suggested that highly refined diets/low fiber diets may increase risk of CD over time. Despite the mixed population level data, individual patients can feel strongly that specific foods increase or decrease their abdominal symptoms. While it is unclear what role dietary fiber has in the management of CD/IBD, for this patient a high fiber diet improved his symptom management enough that he was lost to follow-up by the gastroenterology clinic.
Disclosures:
Erin L. Currey, MD1, Michael Brazeau, DO1, Christopher Casaccio, DO2. P0997 - “Orange” You Glad It Wasn’t Jaundice? Carotenemia due to Dietary Modifications to Manage Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Wright Patterson Medical Center, Wright-Patterson AFB, OH; 2Wright-Patterson Medical Center, Wright-Patterson AFB, OH
Introduction: This case report highlights a patient with Crohn’s disease (CD) who was initially lost to follow-up due to self-management of symptoms with high dietary fiber intake, who’s second presentation to care was to the emergency department with painless “jaundice” ultimately found to be hypercarotenemia from excessive carrot intake.
Case Description/Methods: Patient is an active-duty male with a family history of pancreatic cancer and celiac disease who presented to the ER for fatigue, 10lbs of unintentional weight loss over three months, dark stools without blood, and painless “jaundice.” Labs were remarkable for leukopenia, macrocytic anemia, AST 67, ALT 80, GGT 146, and normal total and direct bilirubin. CT abdomen and pelvis was without acute intrabdominal process. With additional history, it was found that patient was consuming a minimum of half a pound of carrots daily to control his long-standing diarrhea and abdominal pain, leading to a presumptive diagnosis of hypercarotinemia. Vitamin A level was 74.5 ug/dL (H). Of note, patient had previously been evaluated for colitis approximately five years prior. Initial colonoscopy was suspicious but not diagnostic for Crohn’s disease, and the patient was instructed to return for repeat colonoscopy to document chronicity. However, he was lost to follow up for several years and self-titrated his dietary fiber intake to improve his symptoms. Patient now has substantially improved on vedolizumab and skin discoloration improved with reduction in carrot intake.
Discussion: This case highlights an atypical cause of painless “jaundice” and the substantial dietary modifications that patients with IBD often take to manage their abdominal symptoms. Several studies including a Cochrane review and a systematic review in Nutrients have looked into the role of dietary fiber in both the pathogenesis and management of IBD. However, findings from both were limited by inclusion of multiple subtypes of IBD, inadequate power, and high risk for bias. However, epidemiologic studies have suggested that highly refined diets/low fiber diets may increase risk of CD over time. Despite the mixed population level data, individual patients can feel strongly that specific foods increase or decrease their abdominal symptoms. While it is unclear what role dietary fiber has in the management of CD/IBD, for this patient a high fiber diet improved his symptom management enough that he was lost to follow-up by the gastroenterology clinic.
Disclosures:
Erin Currey indicated no relevant financial relationships.
Michael Brazeau indicated no relevant financial relationships.
Christopher Casaccio indicated no relevant financial relationships.
Erin L. Currey, MD1, Michael Brazeau, DO1, Christopher Casaccio, DO2. P0997 - “Orange” You Glad It Wasn’t Jaundice? Carotenemia due to Dietary Modifications to Manage Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

