Sunday Poster Session
Category: IBD
P0910 - Post-Operative Outcomes of Crohn's Disease Patients Undergoing Permanent Ostomy Surgery: Insights from the Cleveland Clinic Inflammatory Bowel Disease Ostomy Research Registry
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Wesam Aleyadeh, MD
Cleveland Clinic Akron General
Akron, OH
Presenting Author(s)
Wesam Aleyadeh, MD1, Raj Jessica Thomas, MD1, Katherine Falloon, MD2, Catherine Larson, MS3, Yueqi (Renee) Wu, MPH4, Qijun Yang, MS5, Florian Rieder, MD6, Suha Abushamma, MD5
1Cleveland Clinic Akron General, Akron, OH; 2Cleveland Clinic Foundation, Shaker Heights, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Cleveland Clinic Lerner Research Institute, Cleveland Heights, OH; 5Cleveland Clinic, Cleveland, OH; 6Digestive Diseases and Surgery Institute; Lerner Research Institute, Program for Global Translational Inflammatory Bowel Diseases; Cleveland Clinic Foundation, Cleveland, OH
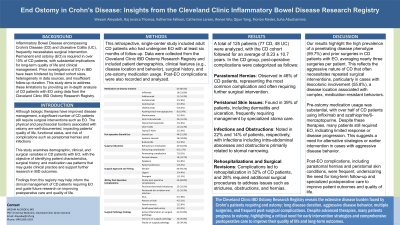
Introduction: Inflammatory Bowel Disease (IBD) and its two distinct forms, ulcerative colitis (UC) and Crohn's disease (CD), often results in the need for surgical intervention. Creation of a permanent end ostomy (EO) is required in some of these patients with a significant impact on patient quality of life and clinical management. This study aims to provide detailed descriptive data on CD patients at the time of ostomy surgery and to report 30-day post-operative complications using data from the Cleveland Clinic IBD Ostomy Research Registry.
Methods: This is a retrospective single-institution study using the first ever comprehensive registry comprising IBD patients with EO created at age 18 or older with at least 6 months of follow-up after EO. Data was collected on various demographic, clinical, and surgical variables. Analysis was conducted using R Studio.
Results: 125 patients (77 CD, 48 UC) were included. In the CD cohort, 75 (97.4%) had end-ileostomy, while 2 had end-colostomy. The mean time from ostomy surgery to the last follow-up was 8.23 (±10.7). The mean age at diagnosis was 28.4 (±16.9) years, and the mean age at ostomy surgery was 41.4 (±15.5) years. The median time from diagnosis to surgery was 13.0 (±10.5) years. The most common indication for surgery was refractory disease (54.5%). Surgeries were most commonly elective in 64 (94.1%) patients with a laparoscopic approach in 44 (65.7%). 61 (91.0%) of patients had evidence of active inflammation on pathology, while 24 (35.8%) and 23 (34.3%) patients had evidence of strictures and enterocutaneous fistulas, respectively. Pre-operative medications were used by 80.5% of patients, most commonly tumor necrosis factor (TNF) blockers, most commonly adalimumab in 11 (14.3%) and infliximab in 10 (13.0%) patients. Peri-operative steroid use was documented in 40 (51.9%) of patients. Thirty-day post-operative complications were observed in 68.8% of patients, most commonly fluid and electrolyte imbalances (32.5%) and peristomal skin irritation and infection (14.3%).
Discussion: This study provides a comprehensive overview of the characteristics and post-operative outcomes of CD patients undergoing ostomy surgery, highlighting significant peri-operative steroid use and a high rate of 30-day post-operative complications. The findings from this registry underscore the complexity of managing CD patients requiring EO and emphasize the need for careful peri-operative management and long-term follow-up to improve patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Wesam Aleyadeh, MD1, Raj Jessica Thomas, MD1, Katherine Falloon, MD2, Catherine Larson, MS3, Yueqi (Renee) Wu, MPH4, Qijun Yang, MS5, Florian Rieder, MD6, Suha Abushamma, MD5. P0910 - Post-Operative Outcomes of Crohn's Disease Patients Undergoing Permanent Ostomy Surgery: Insights from the Cleveland Clinic Inflammatory Bowel Disease Ostomy Research Registry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Akron General, Akron, OH; 2Cleveland Clinic Foundation, Shaker Heights, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Cleveland Clinic Lerner Research Institute, Cleveland Heights, OH; 5Cleveland Clinic, Cleveland, OH; 6Digestive Diseases and Surgery Institute; Lerner Research Institute, Program for Global Translational Inflammatory Bowel Diseases; Cleveland Clinic Foundation, Cleveland, OH
Introduction: Inflammatory Bowel Disease (IBD) and its two distinct forms, ulcerative colitis (UC) and Crohn's disease (CD), often results in the need for surgical intervention. Creation of a permanent end ostomy (EO) is required in some of these patients with a significant impact on patient quality of life and clinical management. This study aims to provide detailed descriptive data on CD patients at the time of ostomy surgery and to report 30-day post-operative complications using data from the Cleveland Clinic IBD Ostomy Research Registry.
Methods: This is a retrospective single-institution study using the first ever comprehensive registry comprising IBD patients with EO created at age 18 or older with at least 6 months of follow-up after EO. Data was collected on various demographic, clinical, and surgical variables. Analysis was conducted using R Studio.
Results: 125 patients (77 CD, 48 UC) were included. In the CD cohort, 75 (97.4%) had end-ileostomy, while 2 had end-colostomy. The mean time from ostomy surgery to the last follow-up was 8.23 (±10.7). The mean age at diagnosis was 28.4 (±16.9) years, and the mean age at ostomy surgery was 41.4 (±15.5) years. The median time from diagnosis to surgery was 13.0 (±10.5) years. The most common indication for surgery was refractory disease (54.5%). Surgeries were most commonly elective in 64 (94.1%) patients with a laparoscopic approach in 44 (65.7%). 61 (91.0%) of patients had evidence of active inflammation on pathology, while 24 (35.8%) and 23 (34.3%) patients had evidence of strictures and enterocutaneous fistulas, respectively. Pre-operative medications were used by 80.5% of patients, most commonly tumor necrosis factor (TNF) blockers, most commonly adalimumab in 11 (14.3%) and infliximab in 10 (13.0%) patients. Peri-operative steroid use was documented in 40 (51.9%) of patients. Thirty-day post-operative complications were observed in 68.8% of patients, most commonly fluid and electrolyte imbalances (32.5%) and peristomal skin irritation and infection (14.3%).
Discussion: This study provides a comprehensive overview of the characteristics and post-operative outcomes of CD patients undergoing ostomy surgery, highlighting significant peri-operative steroid use and a high rate of 30-day post-operative complications. The findings from this registry underscore the complexity of managing CD patients requiring EO and emphasize the need for careful peri-operative management and long-term follow-up to improve patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Wesam Aleyadeh indicated no relevant financial relationships.
Raj Jessica Thomas indicated no relevant financial relationships.
Katherine Falloon: Janssen – Advisory Committee/Board Member. Pfizer – Grant/Research Support.
Catherine Larson indicated no relevant financial relationships.
Yueqi (Renee) Wu indicated no relevant financial relationships.
Qijun Yang indicated no relevant financial relationships.
Florian Rieder: 89Bio – Consultant. AbbVie – Consultant, Grant/Research Support. Adiso – Consultant. Adnovate – Consultant. Agomab – Consultant. Allergan – Advisory Committee/Board Member, Consultant. Arena – Advisory Committee/Board Member, Consultant. AstraZeneca – Advisory Committee/Board Member, Consultant. Bausch & Lomb – Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant, Grant/Research Support. CDISC – Consultant. Celgene/BMS – Advisory Committee/Board Member, Consultant, Grant/Research Support. Celltrion – Consultant. Celsius – Consultant. Cowen – Consultant. Eugit – Consultant. Ferring – Consultant. Galapagos – Consultant. Galmed – Consultant. Genentech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant, Grant/Research Support. Gossamer – Consultant. Granite – Consultant. Guidepoint – Consultant. Helmsley – Consultant. Horizon Therapeutics – Consultant. Image Analysis Limited – Consultant. Index Pharma – Consultant. Jannsen – Consultant. Koutif – Consultant. Landos – Consultant. Mestag – Consultant. Metacrine – Consultant. Mirum – Consultant. Mopec – Consultant. Morphic – Consultant. Myka Labs – Consultant. Organovo – Consultant. Origo – Consultant. Palisade Bio – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support. Pliant – Consultant. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Receptos – Consultant. RedX – Advisory Committee/Board Member, Consultant. Roche – Advisory Committee/Board Member, Consultant. Samsung – Advisory Committee/Board Member, Consultant. Sanofi – Consultant. Surmodics – Consultant. Surrozen – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support. Techlab – Consultant. Teva – Consultant. Theravance – Consultant. Thetis – Consultant. Trix Bio – Consultant. UCB – Advisory Committee/Board Member, Consultant, Grant/Research Support. Ysios – Consultant.
Suha Abushamma indicated no relevant financial relationships.
Wesam Aleyadeh, MD1, Raj Jessica Thomas, MD1, Katherine Falloon, MD2, Catherine Larson, MS3, Yueqi (Renee) Wu, MPH4, Qijun Yang, MS5, Florian Rieder, MD6, Suha Abushamma, MD5. P0910 - Post-Operative Outcomes of Crohn's Disease Patients Undergoing Permanent Ostomy Surgery: Insights from the Cleveland Clinic Inflammatory Bowel Disease Ostomy Research Registry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
