Sunday Poster Session
Category: IBD
P0915 - Inflammatory Bowel Disease (IBD)-Associated Peripheral Arthritis is Not Associated With Objective Markers of Luminal IBD Disease Activity - Results From the CHASE Cohort
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Katherine Falloon, MD
Cleveland Clinic Foundation
Shaker Heights, OH
Presenting Author(s)
Award: Presidential Poster Award
Katherine Falloon, MD1, Suha Abushamma, MD2, Ashwin Ananthakrishnan, MBBS, MPH3, Edward Barnes, MD, MPH, FACG4, Abhik Bhattacharya, MD5, Raymond K. Cross, MD, MS, FACG6, Shashank Cheemalavagu, MD7, Jean-Frédéric Colombel, MD5, Emily Gore, MD5, Hans Herfarth, MD, PhD8, Sara N. Horst, MD9, Jason K. Hou, MD, MS, FACG10, M. Elaine. Husni, MD, MPH7, Jeremy A. Klein, MD11, Edward V. Loftus, MD, FACG12, Dana J. Lukin, MD13, David T.. Rubin, MD, FACG14, Ellen Scherl, MD15, Taha Qazi, MD16, Qijun Yang, MS2, Benjamin L. Cohen, MD7, Brian G.. Feagan, MD17, Florian Rieder, MD18
1Cleveland Clinic Foundation, Shaker Heights, OH; 2Cleveland Clinic, Cleveland, OH; 3Massachusetts General Hospital, Boston, MA; 4University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 5Icahn School of Medicine at Mount Sinai, New York, NY; 6Melissa L. Posner Institute for Digestive Health & Liver Disease at Mercy Medical Center, Baltimore, MD; 7Cleveland Clinic Foundation, Cleveland, OH; 8University of North Carolina at Chapel Hill, Chapel Hill, NC; 9Vanderbilt Inflammatory Bowel Disease Clinic, Nashville, TN; 10Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX; 11University of Chicago Medical Center, Chicago, IL; 12Mayo Clinic College of Medicine and Science, Rochester, MN; 13Jill Roberts Center for Inflammatory Bowel Disease, New York Presbyterian Hospital-Weill Cornell Medicine, New York, NY; 14University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 15New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 16Cleveland Clinic Foundation, Beachwood, OH; 17Western University, London, ON, Canada; 18Digestive Diseases and Surgery Institute; Lerner Research Institute, Program for Global Translational Inflammatory Bowel Diseases; Cleveland Clinic Foundation, Cleveland, OH
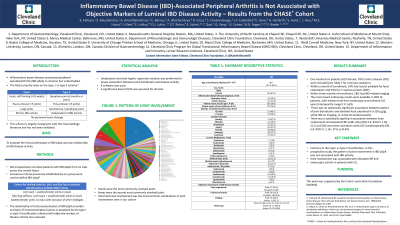
Introduction: Inflammatory bowel disease (IBD)-associated peripheral spondyloarthritis (IBD-pSpA) is common but remains understudied. Although the type I vs type II classification, which categorizes patients based upon number and size of involved joints, is commonly accepted by gastroenterologists, this schema is neither widely accepted within the rheumatology literature nor prospectively validated. The aim of this study was to assess the association between clinical presentation of IBD-pSpA and IBD activity.
Methods: We prospectively recruited patients with IBD-pSpA, defined by previously established consensus criteria (incorporating presence of swollen/tender joints on physical exam), from six sites across the United States. The relationship of clinical presentation of IBD-pSpA (number and type of involved peripheral joints as proposed by the type I vs type II classification schema) with objective markers of disease activity was assessed. Unadjusted univariate logistic regression analysis was performed to assess association between joint distribution and disease activity. R software was used. A significance level of 0.05 was assumed for all tests.
Results: One hundred six patients (61% female, 70% Crohn’s disease (CD)) were included (see Table 1 for summary statistics). Within a month of enrollment, 24% had results available for fecal calprotectin and 53% for C-reactive protein (CRP). Within three months of enrollment, 18% had IBD-related imaging. The most recent endoscopy results were available in 96% of patients, with median time from endoscopy to enrollment 0.8 years (interquartile range 0.3-1.60). There was no statistically significant association between pattern of joint distribution and elevated fecal calprotectin ( >150 μg/g), active IBD on imaging, or active CD endoscopically. There was a statistically significant association between knee involvement and elevated CRP (odds ratio [OR], 4.3; 95% CI, 1.18–21.0; p=0.04) and active ulcerative colitis (UC) endoscopically (OR, 5.9; 95% CI, 1.16– 37.0; p=0.04).
Discussion: Contrary to the type I vs type II classification, in this prospective study, the pattern of joint involvement in IBD-pSpA was not associated with IBD activity. Knee involvement was associated with elevated CRP and endoscopic activity in patients with UC.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Katherine Falloon, MD1, Suha Abushamma, MD2, Ashwin Ananthakrishnan, MBBS, MPH3, Edward Barnes, MD, MPH, FACG4, Abhik Bhattacharya, MD5, Raymond K. Cross, MD, MS, FACG6, Shashank Cheemalavagu, MD7, Jean-Frédéric Colombel, MD5, Emily Gore, MD5, Hans Herfarth, MD, PhD8, Sara N. Horst, MD9, Jason K. Hou, MD, MS, FACG10, M. Elaine. Husni, MD, MPH7, Jeremy A. Klein, MD11, Edward V. Loftus, MD, FACG12, Dana J. Lukin, MD13, David T.. Rubin, MD, FACG14, Ellen Scherl, MD15, Taha Qazi, MD16, Qijun Yang, MS2, Benjamin L. Cohen, MD7, Brian G.. Feagan, MD17, Florian Rieder, MD18. P0915 - Inflammatory Bowel Disease (IBD)-Associated Peripheral Arthritis is Not Associated With Objective Markers of Luminal IBD Disease Activity - Results From the CHASE Cohort, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Katherine Falloon, MD1, Suha Abushamma, MD2, Ashwin Ananthakrishnan, MBBS, MPH3, Edward Barnes, MD, MPH, FACG4, Abhik Bhattacharya, MD5, Raymond K. Cross, MD, MS, FACG6, Shashank Cheemalavagu, MD7, Jean-Frédéric Colombel, MD5, Emily Gore, MD5, Hans Herfarth, MD, PhD8, Sara N. Horst, MD9, Jason K. Hou, MD, MS, FACG10, M. Elaine. Husni, MD, MPH7, Jeremy A. Klein, MD11, Edward V. Loftus, MD, FACG12, Dana J. Lukin, MD13, David T.. Rubin, MD, FACG14, Ellen Scherl, MD15, Taha Qazi, MD16, Qijun Yang, MS2, Benjamin L. Cohen, MD7, Brian G.. Feagan, MD17, Florian Rieder, MD18
1Cleveland Clinic Foundation, Shaker Heights, OH; 2Cleveland Clinic, Cleveland, OH; 3Massachusetts General Hospital, Boston, MA; 4University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 5Icahn School of Medicine at Mount Sinai, New York, NY; 6Melissa L. Posner Institute for Digestive Health & Liver Disease at Mercy Medical Center, Baltimore, MD; 7Cleveland Clinic Foundation, Cleveland, OH; 8University of North Carolina at Chapel Hill, Chapel Hill, NC; 9Vanderbilt Inflammatory Bowel Disease Clinic, Nashville, TN; 10Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX; 11University of Chicago Medical Center, Chicago, IL; 12Mayo Clinic College of Medicine and Science, Rochester, MN; 13Jill Roberts Center for Inflammatory Bowel Disease, New York Presbyterian Hospital-Weill Cornell Medicine, New York, NY; 14University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 15New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 16Cleveland Clinic Foundation, Beachwood, OH; 17Western University, London, ON, Canada; 18Digestive Diseases and Surgery Institute; Lerner Research Institute, Program for Global Translational Inflammatory Bowel Diseases; Cleveland Clinic Foundation, Cleveland, OH
Introduction: Inflammatory bowel disease (IBD)-associated peripheral spondyloarthritis (IBD-pSpA) is common but remains understudied. Although the type I vs type II classification, which categorizes patients based upon number and size of involved joints, is commonly accepted by gastroenterologists, this schema is neither widely accepted within the rheumatology literature nor prospectively validated. The aim of this study was to assess the association between clinical presentation of IBD-pSpA and IBD activity.
Methods: We prospectively recruited patients with IBD-pSpA, defined by previously established consensus criteria (incorporating presence of swollen/tender joints on physical exam), from six sites across the United States. The relationship of clinical presentation of IBD-pSpA (number and type of involved peripheral joints as proposed by the type I vs type II classification schema) with objective markers of disease activity was assessed. Unadjusted univariate logistic regression analysis was performed to assess association between joint distribution and disease activity. R software was used. A significance level of 0.05 was assumed for all tests.
Results: One hundred six patients (61% female, 70% Crohn’s disease (CD)) were included (see Table 1 for summary statistics). Within a month of enrollment, 24% had results available for fecal calprotectin and 53% for C-reactive protein (CRP). Within three months of enrollment, 18% had IBD-related imaging. The most recent endoscopy results were available in 96% of patients, with median time from endoscopy to enrollment 0.8 years (interquartile range 0.3-1.60). There was no statistically significant association between pattern of joint distribution and elevated fecal calprotectin ( >150 μg/g), active IBD on imaging, or active CD endoscopically. There was a statistically significant association between knee involvement and elevated CRP (odds ratio [OR], 4.3; 95% CI, 1.18–21.0; p=0.04) and active ulcerative colitis (UC) endoscopically (OR, 5.9; 95% CI, 1.16– 37.0; p=0.04).
Discussion: Contrary to the type I vs type II classification, in this prospective study, the pattern of joint involvement in IBD-pSpA was not associated with IBD activity. Knee involvement was associated with elevated CRP and endoscopic activity in patients with UC.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Katherine Falloon: Janssen – Advisory Committee/Board Member. Pfizer – Grant/Research Support.
Suha Abushamma indicated no relevant financial relationships.
Ashwin Ananthakrishnan: Geneoscopy – Advisor or Review Panel Member.
Edward Barnes: AbbVie, Inc. – Consultant. Boomerang – Consultant. Bristol-Meyers Squibb – Consultant. Direct Biologics – Consultant. Eli Lilly and Company – Advisor or Review Panel Member. Pfizer – Consultant. Target RWE – Consultant.
Abhik Bhattacharya indicated no relevant financial relationships.
Raymond Cross: AbbVie – Consultant. Adiso – Consultant. Bristol Myers Squibb – Consultant. CorEvitas Registry – Scientific co-director. Fresenius Kabi – Consultant. Fzata – Consultant. IBD Education Group – Executive committee member. Janssen – Consultant, Grant/Research Support. Magellan Health – Consultant. Option Care Health – Consultant. Pfizer – Consultant. Pharmacosmos – Consultant. Samsung Bioepis – Consultant. Sandoz – Consultant. Sebela – Consultant. Takeda – Consultant.
Shashank Cheemalavagu indicated no relevant financial relationships.
Jean-Frédéric Colombel: AbbVie – Consultant, Grant/Research Support. Allergan – Consultant. Amgen – Consultant. AnaptysBio – Consultant. Arena Pharmaceuticals – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squib – Consultant, Grant/Research Support. Celgene – Consultant. Celltrion – Consultant. Eli Lilly – Consultant. Enterome – Consultant. Ferring – Consultant. Galmed Research – Consultant. Genentech – Consultant. Genfit – Stock-publicly held company(excluding mutual/index funds). Glaxo Smith Kline – Consultant. Immunic – Consultant. Intestinal Biotech Development – Stock-publicly held company(excluding mutual/index funds). Iterative Scopes – Consultant. Janssen – Consultant, Grant/Research Support. Johnson & Johnson – Consultant, Grant/Research Support. Kaleido Biosciences – Consultant. Landos – Consultant. MedImmune – Consultant. Merck – Consultant. Microba Life Science – Consultant. Novartis – Consultant. Otsuka Pharmaceutical – Consultant. Pfizer – Consultant. PPM Services – Consultant. Protagonist – Consultant. Sanofi – Consultant. Second Genome – Consultant. Seres – Consultant. Shire – Consultant. Takeda – Consultant, Grant/Research Support. Theradiag – Consultant. TiGenix – Consultant. Vifor – Consultant.
Emily Gore indicated no relevant financial relationships.
Hans Herfarth: Celltrion – Advisory Committee/Board Member. ExeGi – Consultant. Fresenius Kabi – Advisory Committee/Board Member. Gilead – Consultant. Janssen – Advisory Committee/Board Member. Novo Nordisk – Grant/Research Support. Pfizer – Grant/Research Support. Ventyx – Consultant.
Sara Horst: AbbVie – Consultant. Bristol Myers Squibb – Consultant. Janssen – Consultant. Pfizer – Consultant. Takeda – Consultant.
Jason Hou: Abbvie – Grant/Research Support. American Regent – Grant/Research Support. Bristol Myers Squibb – Grant/Research Support. Eli-Lilly – Advisor or Review Panel Member, Grant/Research Support. Janssen – Grant/Research Support. Pfizer – Grant/Research Support. Vedanta – Grant/Research Support.
M. Husni: Abbvie – Consultant. BMS – Consultant. Co-Inventor, PASE Questionnaire, Receives Royalties – Intellectual Property/Patents. Eli Lilly – Consultant. Janssen – Consultant. Novartis – Consultant. UCB – Consultant.
Jeremy Klein indicated no relevant financial relationships.
Edward Loftus: AbbVie – Consultant, Grant/Research Support. Amgen – Consultant. Astellas – Consultant. AstraZeneca – Grant/Research Support. Avalo – Consultant. Boehringer Ingelheim – Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support. Celgene – Consultant. Celltrion – Consultant. Eli Lilly – Consultant. Exact Sciences – Stock-publicly held company(excluding mutual/index funds). Fresenius Kabi – Consultant. Genentech – Consultant, Grant/Research Support. Gilead – Consultant, Grant/Research Support. Iota Biosciences – Consultant. Iterative Health – Grant/Research Support. Janssen – Consultant, Grant/Research Support. Merck – Consultant. Morphic Therapeutics – Consultant. Ono Pharma – Consultant. Receptos – Grant/Research Support. Sun Pharma – Consultant. Surrozen – Consultant. Takeda – Consultant, Grant/Research Support. TR1X Bio – Consultant. UCB – Consultant, Grant/Research Support.
Dana J. Lukin: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. AltruBio – Consultant. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol Myers Squibb – Consultant. Eli Lilly – Consultant. Fresenius Kabi – Consultant. Janssen – Consultant, Grant/Research Support, Speakers Bureau. Magellan Health – Consultant. Palatin Technologies – Consultant. Pfizer – Consultant. Prometheus Laboratories – Consultant. PSI – Consultant. Takeda – Consultant, Grant/Research Support.
David Rubin: AbbVie – Consultant. AltruBio – Consultant. Apex – Consultant. Avalo Therapeutics – Consultant. Bausch Health – Consultant. Bristol Myers Squibb – Consultant. Buhlmann Diagnostics Corp – Consultant. Celgene – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health – Board of Directors. Crohn's & Colitis Foundation – Board of Trustees. Douglas Therapeutics – Consultant. Eli Lilly – Consultant. InDex Pharmaceuticals – Consultant. Intouch Group – Consultant. Iterative Health – Consultant. Janssen Pharmaceuticals – Consultant. Odyssey Thera – Consultant. Pfizer – Consultant. Prometheus Biosciences – Consultant. Samsung Neurologica – Consultant. Takeda – Consultant, Grant/Research Support.
Ellen Scherl: Abbvie – Consultant, Speakers Bureau. BMS – Consultant, Speakers Bureau. Johnson and Johnson – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Taha Qazi: Abbvie Biosciences – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. Celgene/BMS – Advisor or Review Panel Member, Speakers Bureau. Janssen – Speakers Bureau. Pfizer – Advisor or Review Panel Member, Advisory Committee/Board Member. Prometheus Biosciences – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant.
Qijun Yang indicated no relevant financial relationships.
Benjamin L. Cohen: Abbvie – Consultant, support and/or funding, Speakers Bureau. Bristol Myers Squibb – support and/or funding. Celgene – support and/or funding. Emmes – Consultant, Speakers Bureau. Janssen – Consultant, support and/or funding, Speakers Bureau. Pfizer – support and/or funding. Takeda – Consultant, Speakers Bureau. Target RWE – Consultant, Speakers Bureau.
Brian Feagan: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau. AbolerIS – Consultant. AgomAB Therapeutics – Consultant. Allianthera – Consultant. Amgen – Advisory Committee/Board Member, Consultant. AnaptysBio – Advisory Committee/Board Member, Consultant. Applied Molecular Transport Inc – Advisory Committee/Board Member, Consultant. Arena Pharma – Consultant. Atomwise – Consultant. Avoro Capital Advisors – Consultant. Axio Research – Advisory Committee/Board Member. BioJamp – Consultant. Biora Therapeutics – Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant. Boxer – Consultant. Celgene/Bristol Myers Squibb – Advisory Committee/Board Member, Consultant. Celsius Therapeutics – Consultant. Connect BioPharma – Consultant, stock or other ownership interest. Cytoki – Consultant. Disc Medicine – Consultant. Duality – Consultant. EcoR1 Capital – Advisory Committee/Board Member, Consultant. Equillium – Consultant. Ermium – Consultant. First Wave – Consultant. First Word Group – Consultant. Galapagos – Consultant. Galen Atlantica – Consultant. Genentech/Roche – Advisory Committee/Board Member, Consultant. Gilead – Consultant. GlaxoSmithKline – Advisory Committee/Board Member, Consultant. Gossamer Pharma – Consultant, Stock Options. Hinge Bio – Consultant. Hot Spot Therapeutics – Consultant. Imhotex – Consultant. Immunic Therapeutics – Consultant. InDex Pharmaceuticals – Advisory Committee/Board Member, Consultant. JAKAcademy – Consultant. Janssen – Advisory Committee/Board Member, Consultant, Speakers Bureau. Japan Tobacco Inc. – Consultant. Kaleido Biosciences – Consultant. L.E.K. Consulting – Consultant. Landos Biopharma – Consultant. Leadiant – Consultant. Lenczner Slaght – Consultant, payment for expert testimony. LifeSci Capital – Consultant. Lilly – Advisory Committee/Board Member, Consultant. Lument AB – Consultant. Millennium – Consultant. MiroBio – Advisory Committee/Board Member, Consultant. Morgan Lewis – Consultant, payment for expert testimony. Morphic Therapeutics – Advisory Committee/Board Member, Consultant. Mylan – Consultant. OM Pharma – Consultant. Origo BioPharma – Advisory Committee/Board Member, Consultant. Orphagen – Consultant. Pandion Therapeutics – Consultant. Pendopharm – Consultant. Pfizer Inc – Advisory Committee/Board Member, Consultant, Grant/Research Support. Play to Know AG – Consultant. Progenity – Advisory Committee/Board Member, Consultant. Prometheus – Advisory Committee/Board Member, Consultant. Protagonist – Consultant. PTM Therapeutics – Consultant. Q32 Bio – Consultant. Rebiotix – Consultant. REDX – Advisory Committee/Board Member, Consultant. Roche – Consultant. Sandoz – Consultant. Sanofi – Advisory Committee/Board Member, Consultant. Seres Therapeutics – Consultant. Silverback Therapeutics – Consultant. Surrozen Inc. – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Speakers Bureau. Teva – Advisory Committee/Board Member, Consultant. Thelium – Consultant. Tigenix – Consultant. Tillotts Pharma – Advisory Committee/Board Member, Consultant. Ventyx Biosciences – Consultant. VHSquared Ltd – Consultant. Viatris – Consultant. Ysios – Consultant. Ysopia – Consultant. Zealand Pharma – Consultant.
Florian Rieder: 89Bio – Consultant. AbbVie – Consultant, Grant/Research Support. Adiso – Consultant. Adnovate – Consultant. Agomab – Consultant. Allergan – Advisory Committee/Board Member, Consultant. Arena – Advisory Committee/Board Member, Consultant. AstraZeneca – Advisory Committee/Board Member, Consultant. Bausch & Lomb – Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant, Grant/Research Support. CDISC – Consultant. Celgene/BMS – Advisory Committee/Board Member, Consultant, Grant/Research Support. Celltrion – Consultant. Celsius – Consultant. Cowen – Consultant. Eugit – Consultant. Ferring – Consultant. Galapagos – Consultant. Galmed – Consultant. Genentech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant, Grant/Research Support. Gossamer – Consultant. Granite – Consultant. Guidepoint – Consultant. Helmsley – Consultant. Horizon Therapeutics – Consultant. Image Analysis Limited – Consultant. Index Pharma – Consultant. Jannsen – Consultant. Koutif – Consultant. Landos – Consultant. Mestag – Consultant. Metacrine – Consultant. Mirum – Consultant. Mopec – Consultant. Morphic – Consultant. Myka Labs – Consultant. Organovo – Consultant. Origo – Consultant. Palisade Bio – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support. Pliant – Consultant. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Receptos – Consultant. RedX – Advisory Committee/Board Member, Consultant. Roche – Advisory Committee/Board Member, Consultant. Samsung – Advisory Committee/Board Member, Consultant. Sanofi – Consultant. Surmodics – Consultant. Surrozen – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support. Techlab – Consultant. Teva – Consultant. Theravance – Consultant. Thetis – Consultant. Trix Bio – Consultant. UCB – Advisory Committee/Board Member, Consultant, Grant/Research Support. Ysios – Consultant.
Katherine Falloon, MD1, Suha Abushamma, MD2, Ashwin Ananthakrishnan, MBBS, MPH3, Edward Barnes, MD, MPH, FACG4, Abhik Bhattacharya, MD5, Raymond K. Cross, MD, MS, FACG6, Shashank Cheemalavagu, MD7, Jean-Frédéric Colombel, MD5, Emily Gore, MD5, Hans Herfarth, MD, PhD8, Sara N. Horst, MD9, Jason K. Hou, MD, MS, FACG10, M. Elaine. Husni, MD, MPH7, Jeremy A. Klein, MD11, Edward V. Loftus, MD, FACG12, Dana J. Lukin, MD13, David T.. Rubin, MD, FACG14, Ellen Scherl, MD15, Taha Qazi, MD16, Qijun Yang, MS2, Benjamin L. Cohen, MD7, Brian G.. Feagan, MD17, Florian Rieder, MD18. P0915 - Inflammatory Bowel Disease (IBD)-Associated Peripheral Arthritis is Not Associated With Objective Markers of Luminal IBD Disease Activity - Results From the CHASE Cohort, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

