Sunday Poster Session
Category: IBD
P0919 - Recurrence of Inflammatory Bowel Disease is Unlikely but Possible After Permanent End-Ileostomy for Ulcerative Colitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Raj Jessica Thomas, MD
Cleveland Clinic Akron General
Akron, OH
Presenting Author(s)
Raj Jessica Thomas, MD1, Wesam Aleyadeh, MD1, Katherine Falloon, MD2, Qijun Yang, MS3, Florian Rieder, MD4, Suha Abushamma, MD3
1Cleveland Clinic Akron General, Akron, OH; 2Cleveland Clinic Foundation, Shaker Heights, OH; 3Cleveland Clinic, Cleveland, OH; 4Digestive Diseases and Surgery Institute; Lerner Research Institute, Program for Global Translational Inflammatory Bowel Diseases; Cleveland Clinic Foundation, Cleveland, OH
Introduction: Inflammatory Bowel Disease (IBD) in its two distinct forms, ulcerative colitis (UC) and Crohn’s Disease (CD), often results in the need for surgical intervention. In 8% of UC patients and over 10% of CD patients creation of a permanent end ostomy is ultimately required. Published studies assessing IBD patients with end ostomy (EO) are based on small retrospective cohort studies with limited follow-up and are heterogenous. The aim of this study was to analyze post-ostomy recurrence of IBD in UC-EO patients seen by imaging, endoscopy and surgery.
Methods: Retrospective single institution study using the first ever comprehensive registry which included IBD patients with EO created at age 18 or older and had at least 6 months of follow up after EO in our center. Data were described using mean and standard deviation for normally distributed continuous variables, while counts and percentages were used for categorical variables. All statistics were performed in R Studio software.
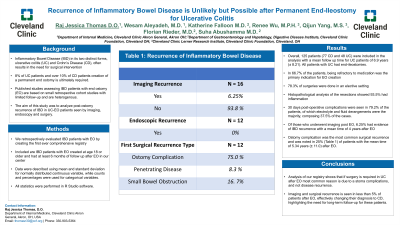
Results: Overall, 125 patients (77 CD and 48 UC) were included in the analysis with a mean follow up time for UC patients of 6.9 years (± 8.21). All patients with UC had end-ileostomies. In 66.7% of the patients, being refractory to medication was the primary indication for end-ileostomy of which 78.3% were done in an elective setting. Pathological analysis showed 93.5% had inflammation on surgical pathology. 30 days post-operative complications were seen in 79.2% of the patients, of which electrolyte and fluid derangements were the majority, composing 37.5% of the cases. Of those who underwent imaging post EO, 6.25% had evidence of IBD recurrence with a mean time of 4 years after EO. Ostomy complication was the most common surgical recurrence and was noted in 25% (Table 1) of patients with the mean time of 5.34 years (± 11.0) after EO.
Discussion: Analysis of our registry shows that if surgery is required in UC after EO, it’s mostly due to a stoma complication, and not due to recurrence. Imaging and surgical recurrence is seen in less than 5% of patients after EO, effectively changing their diagnosis to CD, highlighting the need for long-term follow-up for these patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Raj Jessica Thomas, MD1, Wesam Aleyadeh, MD1, Katherine Falloon, MD2, Qijun Yang, MS3, Florian Rieder, MD4, Suha Abushamma, MD3. P0919 - Recurrence of Inflammatory Bowel Disease is Unlikely but Possible After Permanent End-Ileostomy for Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Akron General, Akron, OH; 2Cleveland Clinic Foundation, Shaker Heights, OH; 3Cleveland Clinic, Cleveland, OH; 4Digestive Diseases and Surgery Institute; Lerner Research Institute, Program for Global Translational Inflammatory Bowel Diseases; Cleveland Clinic Foundation, Cleveland, OH
Introduction: Inflammatory Bowel Disease (IBD) in its two distinct forms, ulcerative colitis (UC) and Crohn’s Disease (CD), often results in the need for surgical intervention. In 8% of UC patients and over 10% of CD patients creation of a permanent end ostomy is ultimately required. Published studies assessing IBD patients with end ostomy (EO) are based on small retrospective cohort studies with limited follow-up and are heterogenous. The aim of this study was to analyze post-ostomy recurrence of IBD in UC-EO patients seen by imaging, endoscopy and surgery.
Methods: Retrospective single institution study using the first ever comprehensive registry which included IBD patients with EO created at age 18 or older and had at least 6 months of follow up after EO in our center. Data were described using mean and standard deviation for normally distributed continuous variables, while counts and percentages were used for categorical variables. All statistics were performed in R Studio software.
Results: Overall, 125 patients (77 CD and 48 UC) were included in the analysis with a mean follow up time for UC patients of 6.9 years (± 8.21). All patients with UC had end-ileostomies. In 66.7% of the patients, being refractory to medication was the primary indication for end-ileostomy of which 78.3% were done in an elective setting. Pathological analysis showed 93.5% had inflammation on surgical pathology. 30 days post-operative complications were seen in 79.2% of the patients, of which electrolyte and fluid derangements were the majority, composing 37.5% of the cases. Of those who underwent imaging post EO, 6.25% had evidence of IBD recurrence with a mean time of 4 years after EO. Ostomy complication was the most common surgical recurrence and was noted in 25% (Table 1) of patients with the mean time of 5.34 years (± 11.0) after EO.
Discussion: Analysis of our registry shows that if surgery is required in UC after EO, it’s mostly due to a stoma complication, and not due to recurrence. Imaging and surgical recurrence is seen in less than 5% of patients after EO, effectively changing their diagnosis to CD, highlighting the need for long-term follow-up for these patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Raj Jessica Thomas indicated no relevant financial relationships.
Wesam Aleyadeh indicated no relevant financial relationships.
Katherine Falloon: Janssen – Advisory Committee/Board Member. Pfizer – Grant/Research Support.
Qijun Yang indicated no relevant financial relationships.
Florian Rieder: 89Bio – Consultant. AbbVie – Consultant, Grant/Research Support. Adiso – Consultant. Adnovate – Consultant. Agomab – Consultant. Allergan – Advisory Committee/Board Member, Consultant. Arena – Advisory Committee/Board Member, Consultant. AstraZeneca – Advisory Committee/Board Member, Consultant. Bausch & Lomb – Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant, Grant/Research Support. CDISC – Consultant. Celgene/BMS – Advisory Committee/Board Member, Consultant, Grant/Research Support. Celltrion – Consultant. Celsius – Consultant. Cowen – Consultant. Eugit – Consultant. Ferring – Consultant. Galapagos – Consultant. Galmed – Consultant. Genentech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant, Grant/Research Support. Gossamer – Consultant. Granite – Consultant. Guidepoint – Consultant. Helmsley – Consultant. Horizon Therapeutics – Consultant. Image Analysis Limited – Consultant. Index Pharma – Consultant. Jannsen – Consultant. Koutif – Consultant. Landos – Consultant. Mestag – Consultant. Metacrine – Consultant. Mirum – Consultant. Mopec – Consultant. Morphic – Consultant. Myka Labs – Consultant. Organovo – Consultant. Origo – Consultant. Palisade Bio – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support. Pliant – Consultant. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Receptos – Consultant. RedX – Advisory Committee/Board Member, Consultant. Roche – Advisory Committee/Board Member, Consultant. Samsung – Advisory Committee/Board Member, Consultant. Sanofi – Consultant. Surmodics – Consultant. Surrozen – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support. Techlab – Consultant. Teva – Consultant. Theravance – Consultant. Thetis – Consultant. Trix Bio – Consultant. UCB – Advisory Committee/Board Member, Consultant, Grant/Research Support. Ysios – Consultant.
Suha Abushamma indicated no relevant financial relationships.
Raj Jessica Thomas, MD1, Wesam Aleyadeh, MD1, Katherine Falloon, MD2, Qijun Yang, MS3, Florian Rieder, MD4, Suha Abushamma, MD3. P0919 - Recurrence of Inflammatory Bowel Disease is Unlikely but Possible After Permanent End-Ileostomy for Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
