Sunday Poster Session
Category: IBD
P0920 - Prevalence of Neurologic Co-Morbidities in Patients with IBD compared to IBS and RA: A Multi-Network Population Based Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Abdullah Mahmood, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Abdullah Mahmood, MD1, Shaina Ailawadi, MD1, Jaime A. Perez, PhD2, Elleson G. Harper, BS1, Edith Y. Ho, MD, MS3, Preetika Sinh, MD4, Vu Q. Nguyen, MD, MS5, Gregory Cooper, MD5, Jeffry Katz, MD5, Fabio Cominelli, MD, PhD5, Miguel D Regueiro, MD6, Emad Mansoor, MD5
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Clinical Research Center, Cleveland, OH; 3Creighton University School of Medicine, Stanford, CA; 4Medical College of Wisconsin, Milwaukee, WI; 5Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 6Cleveland Clinic, Cleveland, OH
Introduction: Extraintestinal manifestations of IBD commonly affect the joints, eyes, and skin. Recent studies have looked at a potential link between IBD and the neurological system, yielding conflicting results. Our study assessed prevalence of common neurological disorders in IBD patients compared to patients with irritable bowel syndrome (IBS), and rheumatoid arthritis (RA), using a large national multicenter cohort.
Methods: We conducted a retrospective study using TriNetX, a de-identified federated database involving 89 healthcare organizations and over 125 million patients. Three cohorts aged ≥ 18 were identified: 1) CD or UC 2) RA only 3) IBS only. We collected demographic data on prevalence of concomitant neurologic co-morbidities (stroke, dementia, multiple sclerosis (MS), epilepsy, Parkinson’s disease (PD), amyotrophic lateral sclerosis (ALS) occurring after the index diagnosis. To control for potential confounding variables, we performed 1:1 greedy nearest neighbor propensity score matching, based on patient demographics and comorbid conditions. We performed independent t-tests for continuous data and chi-square tests for categorical data (presented as frequencies and percentages). We evaluated differences in outcome risk using odds ratios and 95% confidence intervals. All tests were two-tailed with an alpha level of .05.
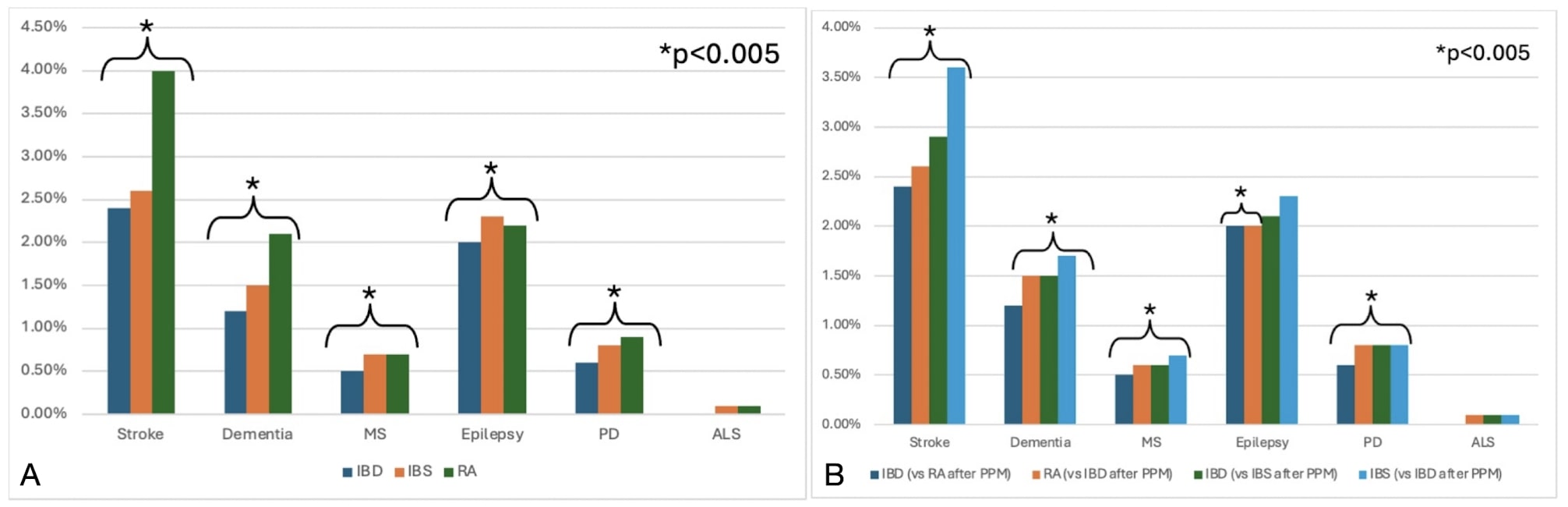
Results: The overall prevalence of MS and ALS in IBD patients was low at 0.5% and 0.02% respectively. After matching for age, race and sex, compared to RA patients, IBD patients exhibited lower prevalence of stroke (OR 0.79 95% CI 0.77, 0.81), dementia (OR 0.88 95% CI 0.85, 0.91), MS (OR 0.85 95% CI 0.81, 0.9), epilepsy (OR 0.89 95% CI 0.87, 0.92), and PD (OR 0.9 95% CI 0.86, 0.95). Compared to IBS patients, IBD patients showed decreased prevalence of stroke (OR 0.92 95% CI 0.9, 0.95), dementia (OR 0.84 95% CI 0.81, 0.87), and PD (OR 0.78 95% CI 0.75, 0.82).
Discussion: Our findings reveal an overall low prevalence of neurologic co-morbidity in IBD compared to IBS and RA, which is reassuring. This could be due to the differing inflammatory profiles, pathophysiologic mechanisms and treatment regimens found in IBD compared to RA and IBS.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abdullah Mahmood, MD1, Shaina Ailawadi, MD1, Jaime A. Perez, PhD2, Elleson G. Harper, BS1, Edith Y. Ho, MD, MS3, Preetika Sinh, MD4, Vu Q. Nguyen, MD, MS5, Gregory Cooper, MD5, Jeffry Katz, MD5, Fabio Cominelli, MD, PhD5, Miguel D Regueiro, MD6, Emad Mansoor, MD5. P0920 - Prevalence of Neurologic Co-Morbidities in Patients with IBD compared to IBS and RA: A Multi-Network Population Based Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Clinical Research Center, Cleveland, OH; 3Creighton University School of Medicine, Stanford, CA; 4Medical College of Wisconsin, Milwaukee, WI; 5Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 6Cleveland Clinic, Cleveland, OH
Introduction: Extraintestinal manifestations of IBD commonly affect the joints, eyes, and skin. Recent studies have looked at a potential link between IBD and the neurological system, yielding conflicting results. Our study assessed prevalence of common neurological disorders in IBD patients compared to patients with irritable bowel syndrome (IBS), and rheumatoid arthritis (RA), using a large national multicenter cohort.
Methods: We conducted a retrospective study using TriNetX, a de-identified federated database involving 89 healthcare organizations and over 125 million patients. Three cohorts aged ≥ 18 were identified: 1) CD or UC 2) RA only 3) IBS only. We collected demographic data on prevalence of concomitant neurologic co-morbidities (stroke, dementia, multiple sclerosis (MS), epilepsy, Parkinson’s disease (PD), amyotrophic lateral sclerosis (ALS) occurring after the index diagnosis. To control for potential confounding variables, we performed 1:1 greedy nearest neighbor propensity score matching, based on patient demographics and comorbid conditions. We performed independent t-tests for continuous data and chi-square tests for categorical data (presented as frequencies and percentages). We evaluated differences in outcome risk using odds ratios and 95% confidence intervals. All tests were two-tailed with an alpha level of .05.
Results: The overall prevalence of MS and ALS in IBD patients was low at 0.5% and 0.02% respectively. After matching for age, race and sex, compared to RA patients, IBD patients exhibited lower prevalence of stroke (OR 0.79 95% CI 0.77, 0.81), dementia (OR 0.88 95% CI 0.85, 0.91), MS (OR 0.85 95% CI 0.81, 0.9), epilepsy (OR 0.89 95% CI 0.87, 0.92), and PD (OR 0.9 95% CI 0.86, 0.95). Compared to IBS patients, IBD patients showed decreased prevalence of stroke (OR 0.92 95% CI 0.9, 0.95), dementia (OR 0.84 95% CI 0.81, 0.87), and PD (OR 0.78 95% CI 0.75, 0.82).
Discussion: Our findings reveal an overall low prevalence of neurologic co-morbidity in IBD compared to IBS and RA, which is reassuring. This could be due to the differing inflammatory profiles, pathophysiologic mechanisms and treatment regimens found in IBD compared to RA and IBS.
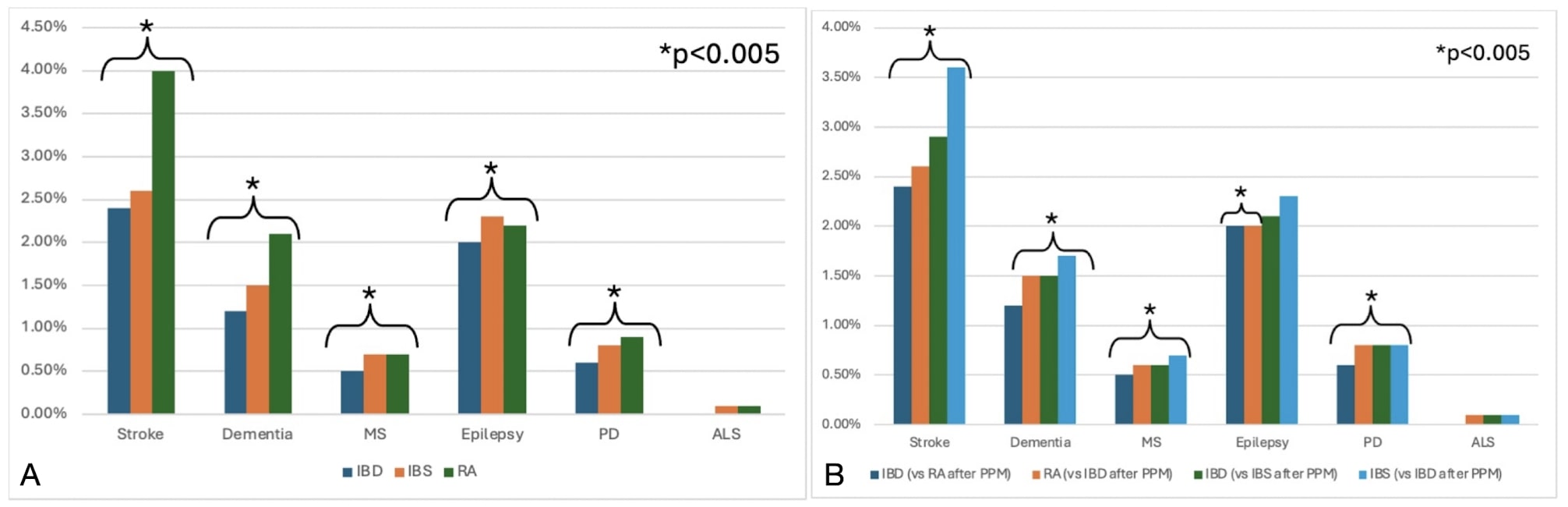
Figure: Graph A: Prevalence of neurological conditions in patients with IBD compared to patients with IBS and patients with RA before propensity score matching (PPM)
Graph B. Prevalence of neurological conditions in patients with IBD compared to patients with IBS and patients with RA after propensity score matching (PPM)
Graph B. Prevalence of neurological conditions in patients with IBD compared to patients with IBS and patients with RA after propensity score matching (PPM)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abdullah Mahmood indicated no relevant financial relationships.
Shaina Ailawadi indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Elleson Harper indicated no relevant financial relationships.
Edith Ho indicated no relevant financial relationships.
Preetika Sinh: Bristol Myers Squibb – Advisory Committee/Board Member.
Vu Nguyen: AbbVie – Speakers Bureau. Eli Lilly – Speakers Bureau.
Gregory Cooper indicated no relevant financial relationships.
Jeffry Katz indicated no relevant financial relationships.
Fabio Cominelli indicated no relevant financial relationships.
Miguel D Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Abdullah Mahmood, MD1, Shaina Ailawadi, MD1, Jaime A. Perez, PhD2, Elleson G. Harper, BS1, Edith Y. Ho, MD, MS3, Preetika Sinh, MD4, Vu Q. Nguyen, MD, MS5, Gregory Cooper, MD5, Jeffry Katz, MD5, Fabio Cominelli, MD, PhD5, Miguel D Regueiro, MD6, Emad Mansoor, MD5. P0920 - Prevalence of Neurologic Co-Morbidities in Patients with IBD compared to IBS and RA: A Multi-Network Population Based Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
