Sunday Poster Session
Category: IBD
P0841 - Ulcerative Colitis in Patients Seen in a Predominantly African American Urban Health Center
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Majd Khadra, MD
Detroit Medical Center/Wayne State University
Detroit, MI
Presenting Author(s)
Majd Khadra, MD1, Anusha Majagi, MD1, Kenan Abou Chaer, MD1, Saumya L. Karne, DO1, Bashar Mohamad, MD2, Paul H. Naylor, PhD3, Milton G. Mutchnick, MD2
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State University, Detroit, MI; 3Wayne State University School of Medicine, Hazel Park, MI
Introduction: Ulcerative colitis (UC) is characterized by inflammation and ulcers in the lining of the colon and rectum. UC may also be more likely diagnosed in non-African Americans as compared to African Americans (AA). However, most of the literature is also based on data from IBD specialty clinics rather than general GI settings. We addressed these issues by evaluating UC in a general GI clinic with a predominately AA population.
Methods: We used ICD-10 codes (K51.9) and electronic medical records to identify first visit patients with UC and a clinic visit between 2018-2020. From a pool of 216 patients using the primary inclusion criteria of endoscopic confirmation of UC, we identified 120 confirmed UC patients. Crohn’s Disease was suspected in 22 patients and 74 patients did not have Inflammatory Bowel Disease. Thus, the accuracy of the ICD-10 coding was 52%. Our data collection included: race, gender, current age, age at diagnosis, colonoscopy with biopsy findings, specialty visit (Gastrointestinal (GI) vs non-GI) and GI follow-up visits thru 2020.
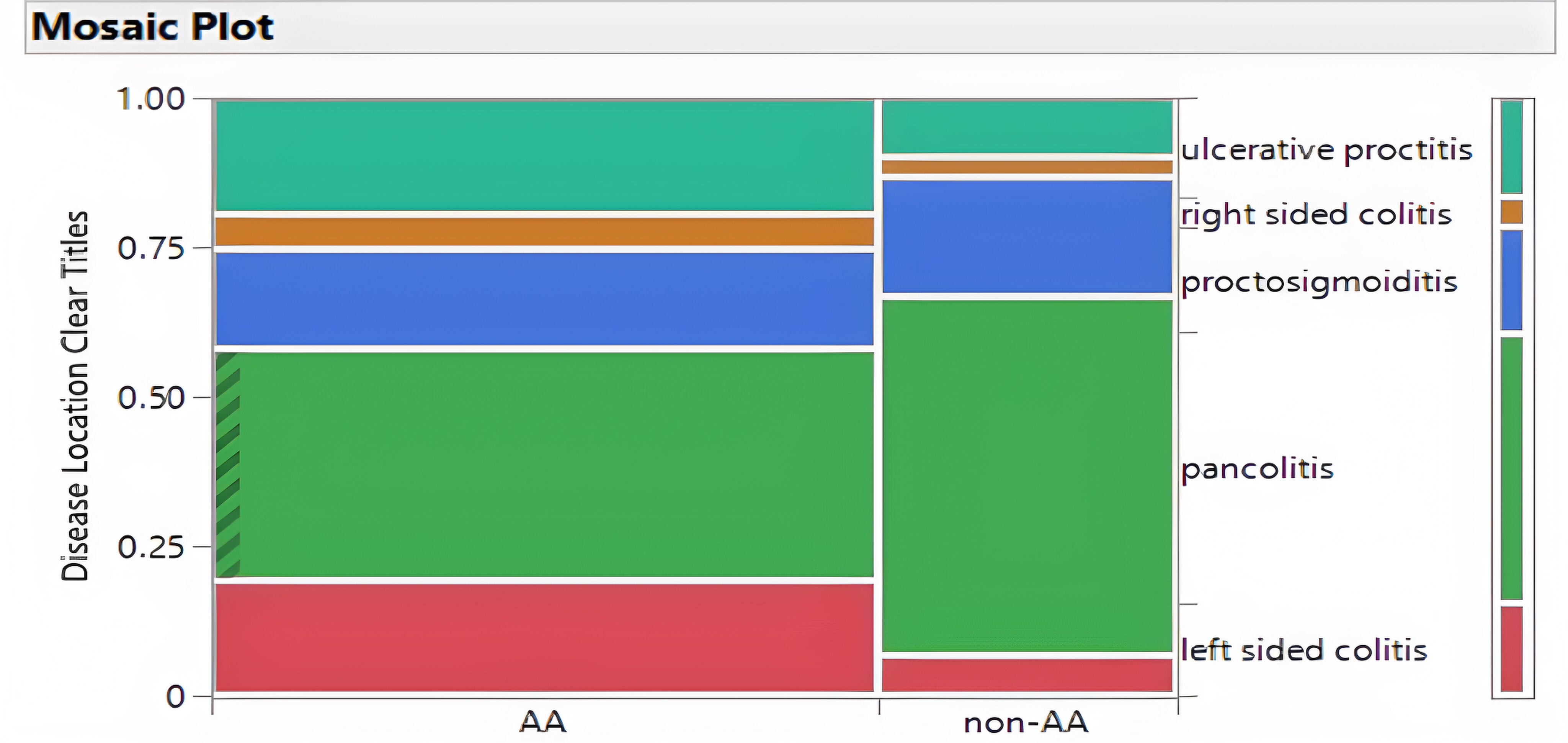
Results: The 120 UC patients were predominately AA (66%), and gender distribution favored females (53% vs 47%; Table 1). The average age at diagnosis/first visit was similar for gender and race. Although many patients were seen by GI physicians (70/120= 58%), significant numbers did not have a GI visit (Table 1). The fact that 23% of patients with endoscopic proven disease documented by a GI consult as inpatients but no clinic visit was unexpected (Table 1). There were notable differences in healthcare utilization among racial groups; African Americans were more likely to be seen by GI physicians (65% vs 46% p=0.047) and had more frequent visits with GI (4 visits vs. 2 visits p=0.014). Racial disparity in the location of disease was noted with AA having more ulcerative proctitis and non-AA higher incidences of pancolitis (Figure 1).
Discussion: Although the racial distribution in the clinics is 70-80%, the 66% AA with UC is consistent with UC being more prevalent in non-AA patients. The two prominent racial differences were higher utilization of GI clinic physicians by AA patients and the location of the primary endoscopic disease as ulcerative proctitis in AA patients as compared to non-AA. The significant numbers of UC patients not seen in the GI clinics suggests that many UC patients are being managed in non-GI settings.
Supported in part by Janssen Scientific Affairs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Majd Khadra, MD1, Anusha Majagi, MD1, Kenan Abou Chaer, MD1, Saumya L. Karne, DO1, Bashar Mohamad, MD2, Paul H. Naylor, PhD3, Milton G. Mutchnick, MD2. P0841 - Ulcerative Colitis in Patients Seen in a Predominantly African American Urban Health Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State University, Detroit, MI; 3Wayne State University School of Medicine, Hazel Park, MI
Introduction: Ulcerative colitis (UC) is characterized by inflammation and ulcers in the lining of the colon and rectum. UC may also be more likely diagnosed in non-African Americans as compared to African Americans (AA). However, most of the literature is also based on data from IBD specialty clinics rather than general GI settings. We addressed these issues by evaluating UC in a general GI clinic with a predominately AA population.
Methods: We used ICD-10 codes (K51.9) and electronic medical records to identify first visit patients with UC and a clinic visit between 2018-2020. From a pool of 216 patients using the primary inclusion criteria of endoscopic confirmation of UC, we identified 120 confirmed UC patients. Crohn’s Disease was suspected in 22 patients and 74 patients did not have Inflammatory Bowel Disease. Thus, the accuracy of the ICD-10 coding was 52%. Our data collection included: race, gender, current age, age at diagnosis, colonoscopy with biopsy findings, specialty visit (Gastrointestinal (GI) vs non-GI) and GI follow-up visits thru 2020.
Results: The 120 UC patients were predominately AA (66%), and gender distribution favored females (53% vs 47%; Table 1). The average age at diagnosis/first visit was similar for gender and race. Although many patients were seen by GI physicians (70/120= 58%), significant numbers did not have a GI visit (Table 1). The fact that 23% of patients with endoscopic proven disease documented by a GI consult as inpatients but no clinic visit was unexpected (Table 1). There were notable differences in healthcare utilization among racial groups; African Americans were more likely to be seen by GI physicians (65% vs 46% p=0.047) and had more frequent visits with GI (4 visits vs. 2 visits p=0.014). Racial disparity in the location of disease was noted with AA having more ulcerative proctitis and non-AA higher incidences of pancolitis (Figure 1).
Discussion: Although the racial distribution in the clinics is 70-80%, the 66% AA with UC is consistent with UC being more prevalent in non-AA patients. The two prominent racial differences were higher utilization of GI clinic physicians by AA patients and the location of the primary endoscopic disease as ulcerative proctitis in AA patients as compared to non-AA. The significant numbers of UC patients not seen in the GI clinics suggests that many UC patients are being managed in non-GI settings.
Supported in part by Janssen Scientific Affairs.
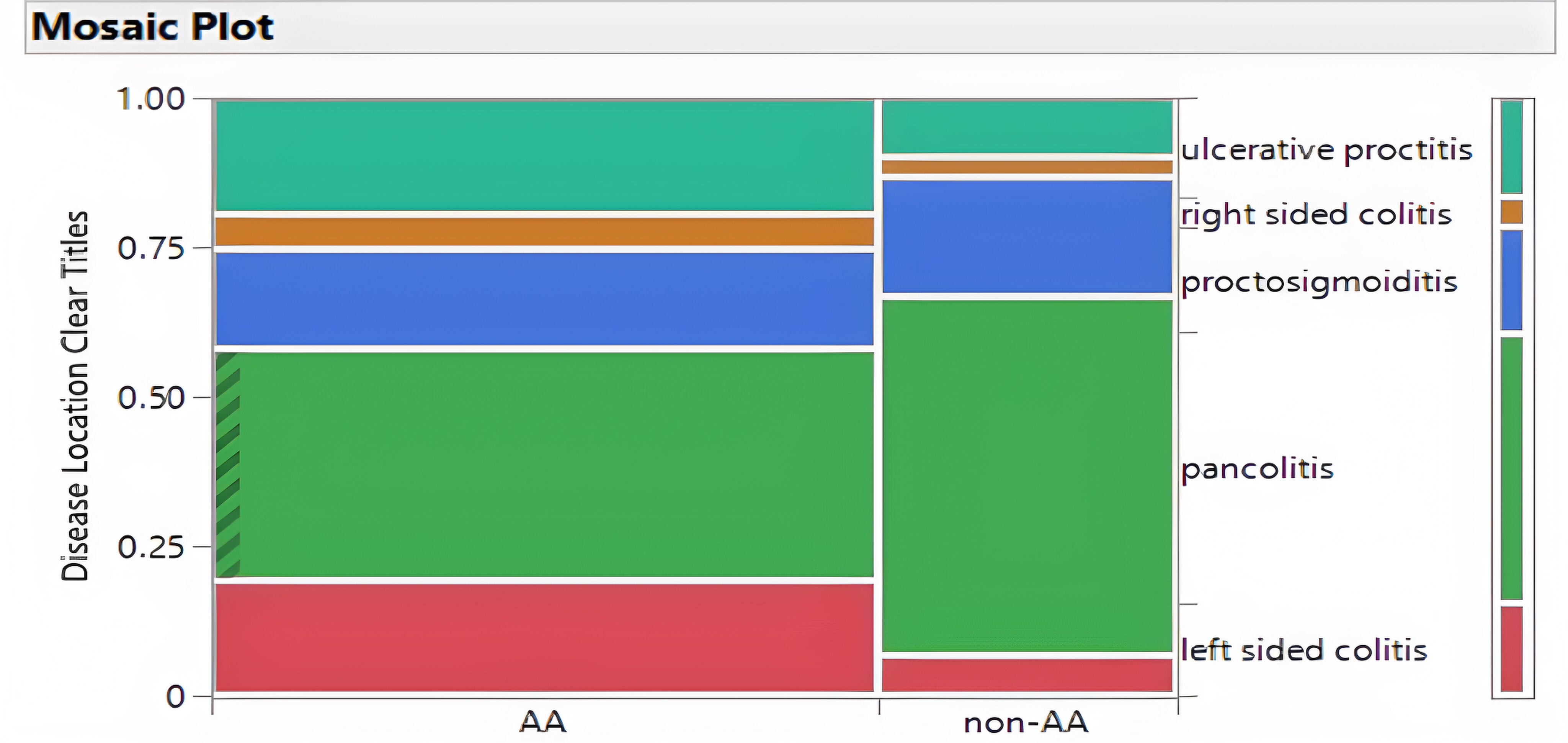
Figure: Figure 1: Racial Disparity in Ulcerative Colitis Disease Location. Ulcerative proctitis was greater in AA than non-AA whereas pancolitis was greater in non-AA as compared to AA.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Majd Khadra indicated no relevant financial relationships.
Anusha Majagi indicated no relevant financial relationships.
Kenan Abou Chaer indicated no relevant financial relationships.
Saumya Karne indicated no relevant financial relationships.
Bashar Mohamad indicated no relevant financial relationships.
Paul Naylor: Janssen Biotech Inc – Grant/Research Support. Salix Pharmaceuticals – Grant/Research Support.
Milton Mutchnick: Janssen – Grant/Research Support. Madrigal – Speakers Bureau. Salix – Grant/Research Support.
Majd Khadra, MD1, Anusha Majagi, MD1, Kenan Abou Chaer, MD1, Saumya L. Karne, DO1, Bashar Mohamad, MD2, Paul H. Naylor, PhD3, Milton G. Mutchnick, MD2. P0841 - Ulcerative Colitis in Patients Seen in a Predominantly African American Urban Health Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
