Sunday Poster Session
Category: GI Bleeding
P0748 - Comparison of Odds of Variceal GI Bleed and Mortality in Inpatients With Alcoholic and Nonalcoholic Liver Cirrhosis After Propensity Score-Matching Using National Inpatient Sample (NIS) Database
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Suman Sharma, MD
Baystate Medical Center
East Longmeadow, MA
Presenting Author(s)
Suman Sharma, MD1, Nilisha Regmi, MD1, Subash Ghimire, MD2
1Baystate Medical Center, East Longmeadow, MA; 2Guthrie Robert Packer Hospital, Sayre, PA
Introduction: Acute variceal upper GI bleed (VUGIB) is a major complication with liver cirrhosis. There is paucity of data in variceal bleeding outcome with different types of cirrhosis. The objective of our study is to compare the rate of VUGIB, odds of mortality (in VUGIB and all-cause), length of hospital stays (LOS), and total cost incurred (TOTCHG) in patients with alcoholic liver cirrhosis (ALC) and non-alcoholic liver cirrhosis (NALC).
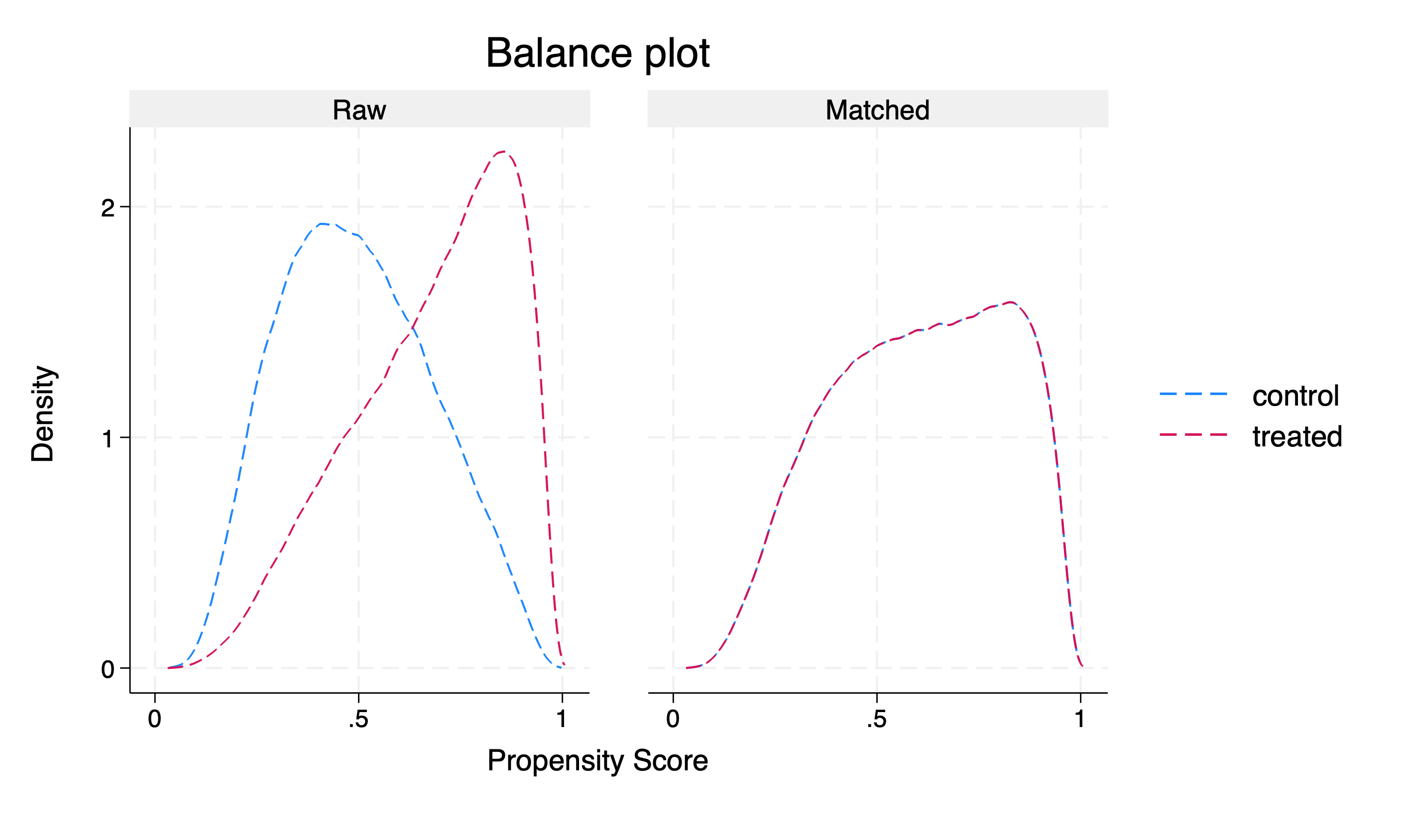
Methods: We used 2016-2019 NIS Databases and ICD-10 CM codes to identify all adults (Age >=18years). Primary diagnosis was defined as VUGIB and Secondary diagnoses as ALC and NALC. ALC patients were matched with NALC patients using propensity scores based on patient’s demographics, hospital characteristics (bed size, teaching, location) and patient’s clinical and Charlson comorbidities. Differences in total LOS, TOTCHG were evaluated using Linear regression and Logistic regression was used to compare odds of in-hospital mortality. STATA 18.0 software was used to evaluate data. ICD-10 codes are as follows: VUGIB-I85.01, I85.11, I86.4, K31.89; ALC- K70.3, K70.2; NALC- K74, K76.1
Results: We identified a total of 233,755 cases of ALC and 359,289 cases of NALC. Post-match, 593,044 observations were noticed in each cohort. The average treatment effect for VUGIB was higher by 0.086% (p=0.014) in NALC as compared to ALC. Inpatient mortality was lower for VUGIB (OR=0.70, p=0.002) as well as for all cause admissions (OR=0.78, p=0.000) for NALC as compared to ALC. LOS was shorter for patients in NALC by 1.11 days (p =0.000) (ALC mean LOS=5.86 days) when admitted for VUGIB and shorter by 3.82 days (p =0.000) (ALC mean LOS=6.52 days) for all-cause admissions. TOTCHG incurred during hospital stay was lower for NALC by $15476.34 (p =0.000) [ALC mean TOTCHG=$84763.93] for VUGIB and lower by $944.93 (p=0.008) [ALC mean TOTCHG=$73548.33] for all- cause admission.
Discussion: Overall, the admissions secondary to VUGIB was higher in NALC patients as compared to ALC patients in the US and it could be the higher sample size of the NALC patient. Surprisingly, the inpatient mortality, length of hospital stay, total cost of hospital stay was lesser both for VUGIB as well as for all-cause admissions in NALC patients as compared to ALC. This could be explained by the shift in the major risk category for the NALC from active viral hepatitis to treated/resolved viral hepatitis leading to stable disease. Further prospective studies are needed to ascertain these important clinical findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Suman Sharma, MD1, Nilisha Regmi, MD1, Subash Ghimire, MD2. P0748 - Comparison of Odds of Variceal GI Bleed and Mortality in Inpatients With Alcoholic and Nonalcoholic Liver Cirrhosis After Propensity Score-Matching Using National Inpatient Sample (NIS) Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baystate Medical Center, East Longmeadow, MA; 2Guthrie Robert Packer Hospital, Sayre, PA
Introduction: Acute variceal upper GI bleed (VUGIB) is a major complication with liver cirrhosis. There is paucity of data in variceal bleeding outcome with different types of cirrhosis. The objective of our study is to compare the rate of VUGIB, odds of mortality (in VUGIB and all-cause), length of hospital stays (LOS), and total cost incurred (TOTCHG) in patients with alcoholic liver cirrhosis (ALC) and non-alcoholic liver cirrhosis (NALC).
Methods: We used 2016-2019 NIS Databases and ICD-10 CM codes to identify all adults (Age >=18years). Primary diagnosis was defined as VUGIB and Secondary diagnoses as ALC and NALC. ALC patients were matched with NALC patients using propensity scores based on patient’s demographics, hospital characteristics (bed size, teaching, location) and patient’s clinical and Charlson comorbidities. Differences in total LOS, TOTCHG were evaluated using Linear regression and Logistic regression was used to compare odds of in-hospital mortality. STATA 18.0 software was used to evaluate data. ICD-10 codes are as follows: VUGIB-I85.01, I85.11, I86.4, K31.89; ALC- K70.3, K70.2; NALC- K74, K76.1
Results: We identified a total of 233,755 cases of ALC and 359,289 cases of NALC. Post-match, 593,044 observations were noticed in each cohort. The average treatment effect for VUGIB was higher by 0.086% (p=0.014) in NALC as compared to ALC. Inpatient mortality was lower for VUGIB (OR=0.70, p=0.002) as well as for all cause admissions (OR=0.78, p=0.000) for NALC as compared to ALC. LOS was shorter for patients in NALC by 1.11 days (p =0.000) (ALC mean LOS=5.86 days) when admitted for VUGIB and shorter by 3.82 days (p =0.000) (ALC mean LOS=6.52 days) for all-cause admissions. TOTCHG incurred during hospital stay was lower for NALC by $15476.34 (p =0.000) [ALC mean TOTCHG=$84763.93] for VUGIB and lower by $944.93 (p=0.008) [ALC mean TOTCHG=$73548.33] for all- cause admission.
Discussion: Overall, the admissions secondary to VUGIB was higher in NALC patients as compared to ALC patients in the US and it could be the higher sample size of the NALC patient. Surprisingly, the inpatient mortality, length of hospital stay, total cost of hospital stay was lesser both for VUGIB as well as for all-cause admissions in NALC patients as compared to ALC. This could be explained by the shift in the major risk category for the NALC from active viral hepatitis to treated/resolved viral hepatitis leading to stable disease. Further prospective studies are needed to ascertain these important clinical findings.
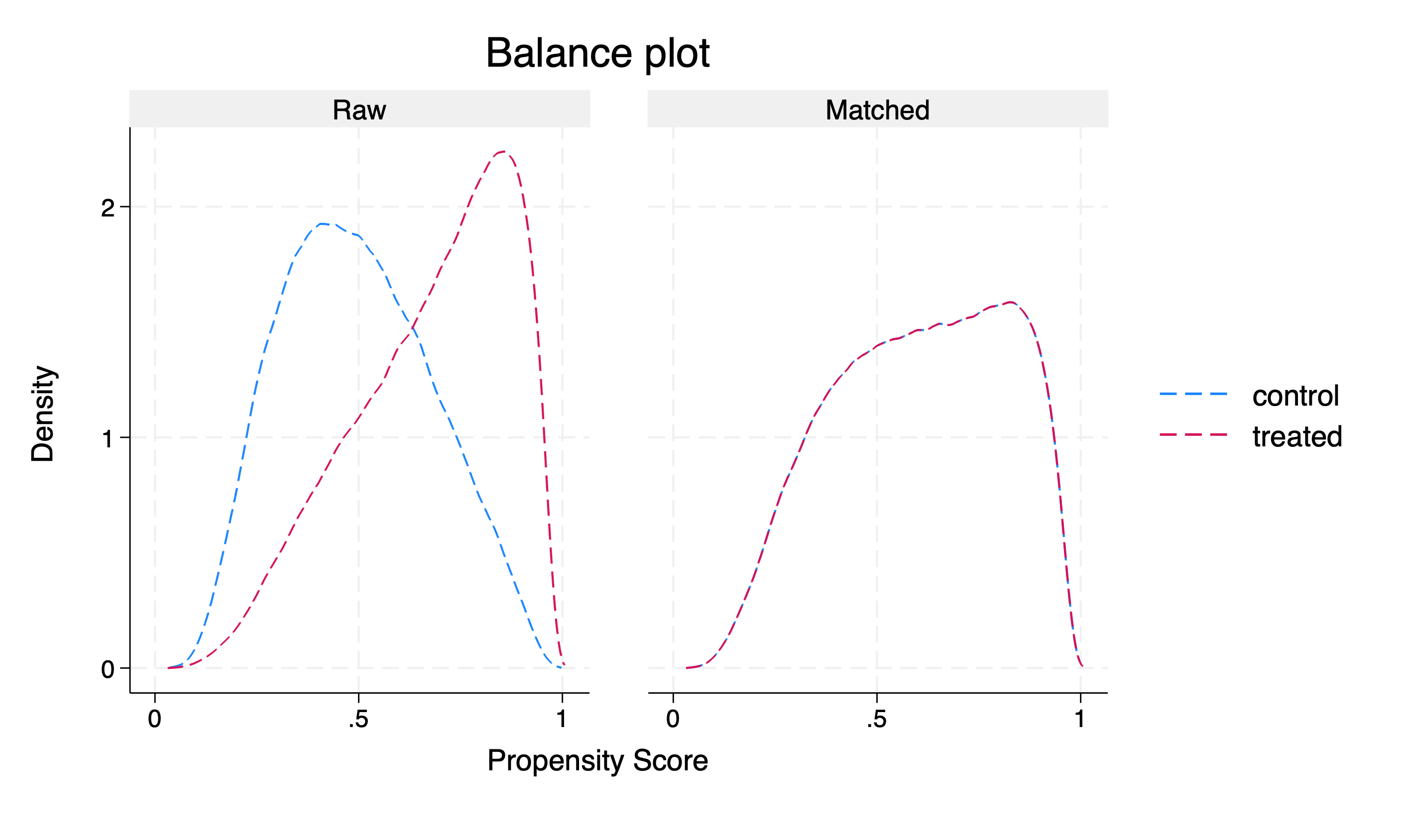
Figure: Density plot depicting the control and the treatment cohort before and after match
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Suman Sharma indicated no relevant financial relationships.
Nilisha Regmi indicated no relevant financial relationships.
Subash Ghimire indicated no relevant financial relationships.
Suman Sharma, MD1, Nilisha Regmi, MD1, Subash Ghimire, MD2. P0748 - Comparison of Odds of Variceal GI Bleed and Mortality in Inpatients With Alcoholic and Nonalcoholic Liver Cirrhosis After Propensity Score-Matching Using National Inpatient Sample (NIS) Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
