Sunday Poster Session
Category: GI Bleeding
P0757 - Acquired Hemophilia A as a Cause of Obscure Gastrointestinal Bleeding
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- LD
Lauren Davis, DO
Lankenau Medical Center
Wynnewood, PA
Presenting Author(s)
Lauren Davis, DO, Erin Hollis, DO, Julianna Tantum, DO, Stephanie Rivera Morales, MD, Nicole Albert, DO
Lankenau Medical Center, Wynnewood, PA
Introduction: Acquired Hemophilia A (AHA) is a rare, acquired bleeding disorder characterized by the production of autoantibodies to clotting Factor VIII. Patients with AHA most often develop spontaneous cutaneous and intramuscular bleeding, though massive gastrointestinal (GI) bleeding has been reported. We present a case of a patient with acute blood loss anemia with recurrent GI bleeding despite multiple unrevealing endoscopic evaluations, ultimately found to have Acquired Hemophilia A.
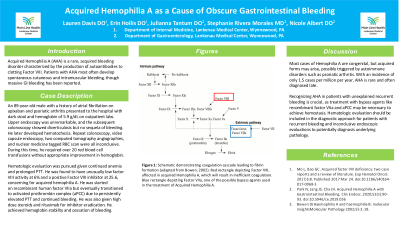
Case Description/Methods: An 89-year-old male with a history of atrial fibrillation on apixaban and psoriatic arthritis presented to the hospital with multiple episodes of dark stool and hemoglobin of 5.9 g/dL on outpatient labs. Upper endoscopy was unremarkable, and the subsequent colonoscopy showed diverticulosis but no sequela of bleeding. He had cessation of dark stool but later developed hematochezia. Further evaluation included repeat colonoscopy, video capsule endoscopy, two computed tomography angiographies, and nuclear medicine tagged RBC scan which were all inconclusive. During this time, he required over 20 red blood cell transfusions without appropriate improvement in hemoglobin.
Hematologic evaluation was pursued given continued anemia and prolonged PTT. The patient was found to have unusually low factor VIII activity at 6% and a positive Factor VIII inhibitor at 25.6, concerning for acquired hemophilia A. He was transferred to an outside facility for recombinant human factor VIIa but eventually transitioned to anti-inhibitor coagulant complex (aPCC) due to persistently elevated PTT and continued bleeding. He was also given high dose steroids and rituximab for inhibitor eradication. He eventually achieved stability of his hemoglobin and cessation of bleeding. However, his course was complicated by respiratory failure secondary to decompensated heart failure, and he transitioned to hospice.
Discussion: Most cases of Hemophilia A are congenital, but acquired forms may arise, possibly triggered by autoimmune disorders such as psoriatic arthritis. With an incidence of only 1.5 cases per million per year, AHA is rare and often diagnosed late. Recognizing AHA in patients with unexplained recurrent bleeding is crucial, as treatment with bypass agents like recombinant factor VIIa and aPCC may be necessary to achieve hemostasis. Hematologic evaluation should be included in the diagnostic approach for patients with recurrent bleeding and inconclusive endoscopic evaluations to potentially diagnosis underlying pathology.
Disclosures:
Lauren Davis, DO, Erin Hollis, DO, Julianna Tantum, DO, Stephanie Rivera Morales, MD, Nicole Albert, DO. P0757 - Acquired Hemophilia A as a Cause of Obscure Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Lankenau Medical Center, Wynnewood, PA
Introduction: Acquired Hemophilia A (AHA) is a rare, acquired bleeding disorder characterized by the production of autoantibodies to clotting Factor VIII. Patients with AHA most often develop spontaneous cutaneous and intramuscular bleeding, though massive gastrointestinal (GI) bleeding has been reported. We present a case of a patient with acute blood loss anemia with recurrent GI bleeding despite multiple unrevealing endoscopic evaluations, ultimately found to have Acquired Hemophilia A.
Case Description/Methods: An 89-year-old male with a history of atrial fibrillation on apixaban and psoriatic arthritis presented to the hospital with multiple episodes of dark stool and hemoglobin of 5.9 g/dL on outpatient labs. Upper endoscopy was unremarkable, and the subsequent colonoscopy showed diverticulosis but no sequela of bleeding. He had cessation of dark stool but later developed hematochezia. Further evaluation included repeat colonoscopy, video capsule endoscopy, two computed tomography angiographies, and nuclear medicine tagged RBC scan which were all inconclusive. During this time, he required over 20 red blood cell transfusions without appropriate improvement in hemoglobin.
Hematologic evaluation was pursued given continued anemia and prolonged PTT. The patient was found to have unusually low factor VIII activity at 6% and a positive Factor VIII inhibitor at 25.6, concerning for acquired hemophilia A. He was transferred to an outside facility for recombinant human factor VIIa but eventually transitioned to anti-inhibitor coagulant complex (aPCC) due to persistently elevated PTT and continued bleeding. He was also given high dose steroids and rituximab for inhibitor eradication. He eventually achieved stability of his hemoglobin and cessation of bleeding. However, his course was complicated by respiratory failure secondary to decompensated heart failure, and he transitioned to hospice.
Discussion: Most cases of Hemophilia A are congenital, but acquired forms may arise, possibly triggered by autoimmune disorders such as psoriatic arthritis. With an incidence of only 1.5 cases per million per year, AHA is rare and often diagnosed late. Recognizing AHA in patients with unexplained recurrent bleeding is crucial, as treatment with bypass agents like recombinant factor VIIa and aPCC may be necessary to achieve hemostasis. Hematologic evaluation should be included in the diagnostic approach for patients with recurrent bleeding and inconclusive endoscopic evaluations to potentially diagnosis underlying pathology.
Disclosures:
Lauren Davis indicated no relevant financial relationships.
Erin Hollis indicated no relevant financial relationships.
Julianna Tantum indicated no relevant financial relationships.
Stephanie Rivera Morales indicated no relevant financial relationships.
Nicole Albert indicated no relevant financial relationships.
Lauren Davis, DO, Erin Hollis, DO, Julianna Tantum, DO, Stephanie Rivera Morales, MD, Nicole Albert, DO. P0757 - Acquired Hemophilia A as a Cause of Obscure Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
