Sunday Poster Session
Category: GI Bleeding
P0760 - Unveiling a Mysterious Case of ATTR Gastrointestinal Amyloidosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Temitope Omoladun-Tijani, MD
Brown Medicine/Lifespan
Providence, RI
Presenting Author(s)
Temitope Omoladun-Tijani, MD1, Vaisali Chilamkurthy, MD1, Steven Moss, MD1, Savan Kothadia, MD2, Eleanor Lewin, MD3, Daniel G. McCall, MD4, Maureen Whittelsey, BS5
1Brown Medicine/Lifespan, Providence, RI; 2Brown University / Lifespan Physician Group, Providence, RI; 3Providence VA Medical Center, Providence, RI; 4Providence VA Medical Center, East Greenwich, RI; 5Warren Alpert Medical School of Brown University, Providence, RI
Introduction: Amyloidosis is characterized by extracellular deposition of amyloid fibrils in various tissues, leading to progressive organ dysfunction. Clinical manifestations of amyloidosis vary based on the organs involved and the type of amyloid protein deposited. Commonly affected organs include the kidneys, heart, liver, and peripheral nerves. The different subtypes of amyloidosis depend on the type of deposited protein, with secondary (AA) amyloidosis being the most common. Other types include primary (AL) and hereditary amyloidosis (ATTR). Diagnosis requires a combination of clinical, laboratory, and histopathological evaluations. Tissue biopsy with Congo red staining showing apple-green birefringence under polarized light remains the gold standard. We present a rare case of ATTR gastrointestinal amyloidosis.
Case Description/Methods: A 58-year-old male with no prior medical history presented with near syncope and lightheadedness for one month and intermittent melena and hematochezia. Exam was significant for hepatomegaly and abdominal tenderness. Notable labs included hemoglobin 7.0 g/dl compared to a baseline of 13.3 g/dl, iron 22 ug/dl, transferrin 344 mg/dl, ferritin 32 ng/ml, alkaline phosphatase of 484 Units/L, and normal liver enzymes.
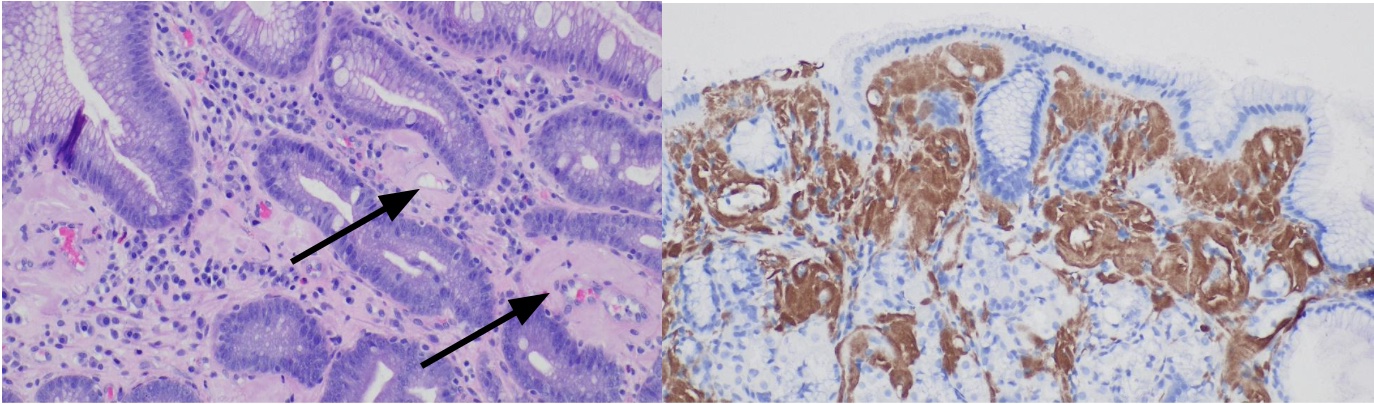
Computed tomography of the abdomen and pelvis showed hepatomegaly. Magnetic resonance cholangiopancreatography showed hepatomegaly AND, several hepatic cysts. Esophagogastroduodenoscopy and colonoscopy revealed no sources of bleeding . Biopsies from gastroesophageal junction, stomach, and duodenum showed significant amyloid deposition. Video capsule endoscopy was performed and showed a large blood clot in the gastric body requiring a second EGD, showing bleeding from the site of gastric biopsies. Further immunohistochemical stains suggested systemic ATTR amyloidosis.
Discussion: This case illustrates the diagnostic challenges of amyloidosis, particularly with atypical presentations such as gastrointestinal bleeding and hepatomegaly. The patient’s nonspecific symptoms of anemia led to a broad workup with the surprising finding of ATTR amyloidosis of the upper GI tract. Gastrointestinal involvement in amyloidosis is rare and often missed. In this case, amyloid infiltration likely caused the vascular fragility and gastrointestinal bleeding. Timely diagnosis through comprehensive evaluation, including tissue biopsy and amyloid typing, is crucial. Recognizing transthyretin-related amyloidosis (ATTR) early can guide appropriate treatment and improve patient outcomes.
Disclosures:
Temitope Omoladun-Tijani, MD1, Vaisali Chilamkurthy, MD1, Steven Moss, MD1, Savan Kothadia, MD2, Eleanor Lewin, MD3, Daniel G. McCall, MD4, Maureen Whittelsey, BS5. P0760 - Unveiling a Mysterious Case of ATTR Gastrointestinal Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown Medicine/Lifespan, Providence, RI; 2Brown University / Lifespan Physician Group, Providence, RI; 3Providence VA Medical Center, Providence, RI; 4Providence VA Medical Center, East Greenwich, RI; 5Warren Alpert Medical School of Brown University, Providence, RI
Introduction: Amyloidosis is characterized by extracellular deposition of amyloid fibrils in various tissues, leading to progressive organ dysfunction. Clinical manifestations of amyloidosis vary based on the organs involved and the type of amyloid protein deposited. Commonly affected organs include the kidneys, heart, liver, and peripheral nerves. The different subtypes of amyloidosis depend on the type of deposited protein, with secondary (AA) amyloidosis being the most common. Other types include primary (AL) and hereditary amyloidosis (ATTR). Diagnosis requires a combination of clinical, laboratory, and histopathological evaluations. Tissue biopsy with Congo red staining showing apple-green birefringence under polarized light remains the gold standard. We present a rare case of ATTR gastrointestinal amyloidosis.
Case Description/Methods: A 58-year-old male with no prior medical history presented with near syncope and lightheadedness for one month and intermittent melena and hematochezia. Exam was significant for hepatomegaly and abdominal tenderness. Notable labs included hemoglobin 7.0 g/dl compared to a baseline of 13.3 g/dl, iron 22 ug/dl, transferrin 344 mg/dl, ferritin 32 ng/ml, alkaline phosphatase of 484 Units/L, and normal liver enzymes.
Computed tomography of the abdomen and pelvis showed hepatomegaly. Magnetic resonance cholangiopancreatography showed hepatomegaly AND, several hepatic cysts. Esophagogastroduodenoscopy and colonoscopy revealed no sources of bleeding . Biopsies from gastroesophageal junction, stomach, and duodenum showed significant amyloid deposition. Video capsule endoscopy was performed and showed a large blood clot in the gastric body requiring a second EGD, showing bleeding from the site of gastric biopsies. Further immunohistochemical stains suggested systemic ATTR amyloidosis.
Discussion: This case illustrates the diagnostic challenges of amyloidosis, particularly with atypical presentations such as gastrointestinal bleeding and hepatomegaly. The patient’s nonspecific symptoms of anemia led to a broad workup with the surprising finding of ATTR amyloidosis of the upper GI tract. Gastrointestinal involvement in amyloidosis is rare and often missed. In this case, amyloid infiltration likely caused the vascular fragility and gastrointestinal bleeding. Timely diagnosis through comprehensive evaluation, including tissue biopsy and amyloid typing, is crucial. Recognizing transthyretin-related amyloidosis (ATTR) early can guide appropriate treatment and improve patient outcomes.
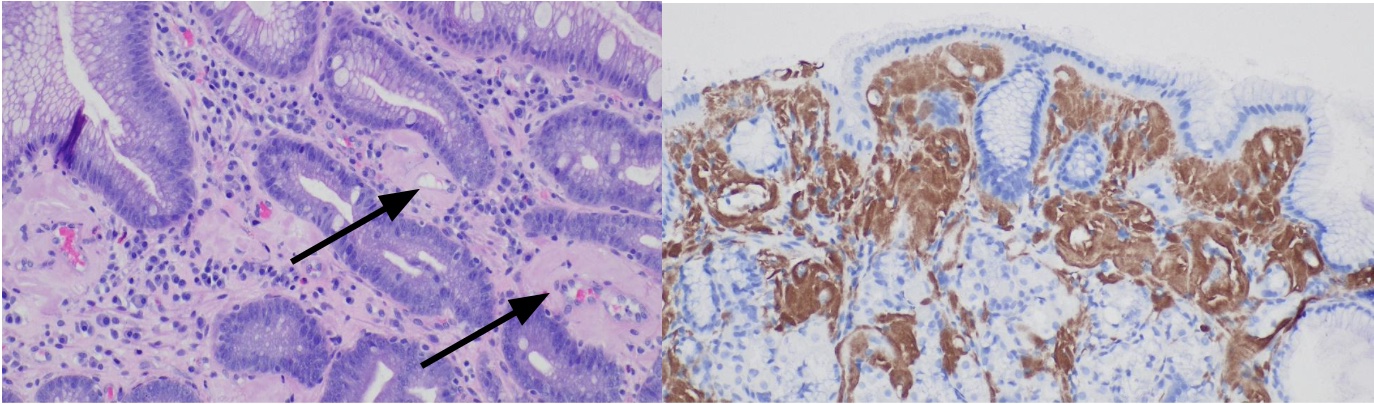
Figure: A. Amyloid in the gastroesophageal junction also with intestinal metaplasia; the amyloid can be seen encircling blood vessels (H&E, 20x)
B. A transthyretin (prealbumin) immunostain highlights the amyloid deposition (IHC, 20x)
B. A transthyretin (prealbumin) immunostain highlights the amyloid deposition (IHC, 20x)
Disclosures:
Temitope Omoladun-Tijani indicated no relevant financial relationships.
Vaisali Chilamkurthy indicated no relevant financial relationships.
Steven Moss indicated no relevant financial relationships.
Savan Kothadia indicated no relevant financial relationships.
Eleanor Lewin indicated no relevant financial relationships.
Daniel McCall indicated no relevant financial relationships.
Maureen Whittelsey indicated no relevant financial relationships.
Temitope Omoladun-Tijani, MD1, Vaisali Chilamkurthy, MD1, Steven Moss, MD1, Savan Kothadia, MD2, Eleanor Lewin, MD3, Daniel G. McCall, MD4, Maureen Whittelsey, BS5. P0760 - Unveiling a Mysterious Case of ATTR Gastrointestinal Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
