Sunday Poster Session
Category: General Endoscopy
P0670 - Clinical Predictive Factors for Endoscopic Findings in Acute Gastrointestinal Bleeding
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpeg.jpg)
Arsh Momin, MD
Penn State Health Milton S. Hershey Medical Center
Atlanta, GA
Presenting Author(s)
Arsh Momin, MD1, Yixuan Du, BS2, Rhea Kanwar, BS2, Erik Lehman, MS2, Kofi Clarke, MD2
1Penn State Health Milton S. Hershey Medical Center, Atlanta, GA; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Gastrointestinal bleeding (GIB) remains a significant cause of morbidity and mortality in the United States. The Glasgow Blatchford Score risk-stratifies patients with upper GIB and can help determine candidates for outpatient management. The AIM65 is a score used for upper gastrointestinal bleeding to determine in-hospital mortality. There are no simple to use scoring systems or predictors that identifies the probability of finding a culprit lesion on endoscopy.
Methods: We performed an initial query using TriNetX and identified patients who met the inclusion criteria of adult patients admitted from 2017 to 2022 within one day of a new diagnosis of Acute Gastrointestinal Bleed (ICD-10 code of K92.2). We excluded duplicate patients, patients with extraluminal causes of gastrointestinal hemorrhage, and patients that did not have an inpatient endoscopy. Data on patients’ demographics, vitals, lab results, transfusion requirements, endoscopic findings were analyzed in depth. Outcomes sought were clinical factors that were predictive of finding a culprit lesion on endoscopy, stigmata of bleeding, and detection of a treatable lesion during endoscopy.
Results: Approximately 535 patients were identified with an initial diagnosis of acute gastrointestinal bleed. A total of 163 unique patients resulted after exclusion of patients with history of gastrointestinal bleeding (GIB), who did not have an inpatient endoscopy, or had an extraluminal source of bleeding.
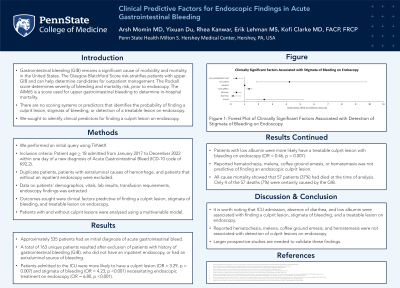
Patients admitted to the ICU were more likely to have a culprit lesion and stigmata of bleeding necessitating endoscopic treatment on endoscopy. Patients with low albumin were more likely have a treatable culprit lesion with bleeding on endoscopy. Reported hematochezia, melena, coffee ground emesis, or hematemesis was not predictive of finding an endoscopic culprit lesion.
All-cause mortality showed that 57 patients (37%) had died at the time of analysis. Only 4 of the 57 deaths (7%) were certainly caused by the GIB.
Discussion: It is worth noting that ICU admission, absence of diarrhea, and low albumin were associated with finding a culprit lesion, stigmata of bleeding, and a treatable lesion on endoscopy. The GBS score was predictive of detection of a treatable lesion on endoscopy. Surprisingly, hematochezia, melena, coffee ground emesis, and hematemesis were not associated with detection of culprit lesions, stigmata of bleeding, or endoscopically treatable lesions. Larger prospective studies are needed to validate these findings.
Disclosures:
Arsh Momin, MD1, Yixuan Du, BS2, Rhea Kanwar, BS2, Erik Lehman, MS2, Kofi Clarke, MD2. P0670 - Clinical Predictive Factors for Endoscopic Findings in Acute Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Atlanta, GA; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Gastrointestinal bleeding (GIB) remains a significant cause of morbidity and mortality in the United States. The Glasgow Blatchford Score risk-stratifies patients with upper GIB and can help determine candidates for outpatient management. The AIM65 is a score used for upper gastrointestinal bleeding to determine in-hospital mortality. There are no simple to use scoring systems or predictors that identifies the probability of finding a culprit lesion on endoscopy.
Methods: We performed an initial query using TriNetX and identified patients who met the inclusion criteria of adult patients admitted from 2017 to 2022 within one day of a new diagnosis of Acute Gastrointestinal Bleed (ICD-10 code of K92.2). We excluded duplicate patients, patients with extraluminal causes of gastrointestinal hemorrhage, and patients that did not have an inpatient endoscopy. Data on patients’ demographics, vitals, lab results, transfusion requirements, endoscopic findings were analyzed in depth. Outcomes sought were clinical factors that were predictive of finding a culprit lesion on endoscopy, stigmata of bleeding, and detection of a treatable lesion during endoscopy.
Results: Approximately 535 patients were identified with an initial diagnosis of acute gastrointestinal bleed. A total of 163 unique patients resulted after exclusion of patients with history of gastrointestinal bleeding (GIB), who did not have an inpatient endoscopy, or had an extraluminal source of bleeding.
Patients admitted to the ICU were more likely to have a culprit lesion and stigmata of bleeding necessitating endoscopic treatment on endoscopy. Patients with low albumin were more likely have a treatable culprit lesion with bleeding on endoscopy. Reported hematochezia, melena, coffee ground emesis, or hematemesis was not predictive of finding an endoscopic culprit lesion.
All-cause mortality showed that 57 patients (37%) had died at the time of analysis. Only 4 of the 57 deaths (7%) were certainly caused by the GIB.
Discussion: It is worth noting that ICU admission, absence of diarrhea, and low albumin were associated with finding a culprit lesion, stigmata of bleeding, and a treatable lesion on endoscopy. The GBS score was predictive of detection of a treatable lesion on endoscopy. Surprisingly, hematochezia, melena, coffee ground emesis, and hematemesis were not associated with detection of culprit lesions, stigmata of bleeding, or endoscopically treatable lesions. Larger prospective studies are needed to validate these findings.
Disclosures:
Arsh Momin indicated no relevant financial relationships.
Yixuan Du indicated no relevant financial relationships.
Rhea Kanwar indicated no relevant financial relationships.
Erik Lehman indicated no relevant financial relationships.
Kofi Clarke: ABBVie – Consultant, Speakers Bureau. Johnson and Johnson – Advisor or Review Panel Member, Speakers Bureau. Pfizer – Consultant. Takeda – Consultant, Speakers Bureau.
Arsh Momin, MD1, Yixuan Du, BS2, Rhea Kanwar, BS2, Erik Lehman, MS2, Kofi Clarke, MD2. P0670 - Clinical Predictive Factors for Endoscopic Findings in Acute Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
