Sunday Poster Session
Category: General Endoscopy
P0678 - Clinical Impact of GLP-1RA On Endoscopy: A Retrospective Cohort Study in Endoscopy Patients
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Braden Kuo, MD, MSc, FACG
Center for Neurointestinal Health, Massachusetts General Hospital
Boston, MA
Presenting Author(s)
Rebecca Karlson, BS1, Jenna Clukey, BA2, Victoria Beck, BA2, Jonathan Kuang Ziyang, MBBS3, Giulia Maria Corradini, MD4, Mia Dekel, 5, Giulia Lojacono, MS6, Akua Nuako, MD1, Blythe Peterson, BA1, Diane Somlo, MD, MBA1, Nir Bar, MD7, Ion Hobai, MD1, Braden Kuo, MD, MSc, FACG2
1Massachusetts General Hospital, Boston, MA; 2Center for Neurointestinal Health, Massachusetts General Hospital, Boston, MA; 3Massachusetts General Hospital, Harvard Medical School, Boston, MA; 4University of Milan, Vedano al Lambro, Lombardia, Italy; 5Humanitas university, Milan, Lombardia, Italy; 6Humanitas University, Milan, Lombardia, Italy; 7MGH, Brookline, MA
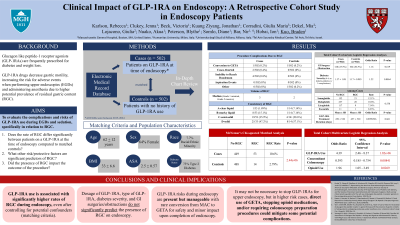
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1RA) are increasingly prescribed for diabetes management and weight loss. GLP-1RA decrease gastric motility, increasing the risk for adverse events in upper endoscopies (UE) due to higher risk of residual gastric content (RGC). This study evaluates the risks of GLP-1RA use during UE and sedation and assesses the impact of diabetes severity, GLP-1RA type, concomitant colonoscopy, and physical health status (ASA) on rates of RGC.
Methods: We identified index cases of patients on GLP-1RA at the time of UE from medical records from 2015-2024. Controls not on GLP-1RA were matched by age (± 5yrs), sex, race, diabetes status, BMI class, and ASA (1-4). Outcomes of interest included presence of RGC (volume and consistency blindly graded by 3 endoscopists), change in anesthesia plan, procedure termination, inability to reach duodenum, and aspiration events. We noted confounders for RGC (gastric surgeries, GI cancers, bowel obstruction) and compared the rates of RGC between cases and controls (Group A includes confounders, Group B excludes confounders). Among cases, we compared rates of RGC between GLP-1RA type, diabetes status and severity, ASA status, and concomitant colonoscopy.
Results: We identified 984 patients: mean age 60yrs, 63% female, 66% obese, and 74% type 2 diabetic. Group A had 581 cases and 403 controls; Group B had 440 cases and 321 controls. RGC rate was significantly higher in cases vs controls for both groups (p< 0.0001). There were no differences in RGC due to GLP-1RA type or diabetes status/severity. Among cases, patients with a low-risk ASA (1,2) and those with concomitant colonoscopy had significantly lower rates of RGC (p< 0.05). There were no complications from RGC in UE among controls. In cases, the rate of complications was low (< 1%). For those who experienced complications, most had a moderate/large amount and a semi-solid/solid consistency of RGC.
Discussion: GLP-1RA use is associated with significantly higher rates of RGC before and after accounting for confounders. Diabetes and type of GLP1-RA did not impact the rate of RGC, but patients having a concomitant colonoscopy and lower anesthetic risk had lower rates of RGC. Overall, GLP-1RA risks during UE are present but manageable with rare conversion to general anesthesia (GA) for safety and minor impact on completion of UE. Our results indicate that it may not be necessary to stop GLP-1RA for UE, but direct use of GA could mitigate complications in higher risk cases.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rebecca Karlson, BS1, Jenna Clukey, BA2, Victoria Beck, BA2, Jonathan Kuang Ziyang, MBBS3, Giulia Maria Corradini, MD4, Mia Dekel, 5, Giulia Lojacono, MS6, Akua Nuako, MD1, Blythe Peterson, BA1, Diane Somlo, MD, MBA1, Nir Bar, MD7, Ion Hobai, MD1, Braden Kuo, MD, MSc, FACG2. P0678 - Clinical Impact of GLP-1RA On Endoscopy: A Retrospective Cohort Study in Endoscopy Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Massachusetts General Hospital, Boston, MA; 2Center for Neurointestinal Health, Massachusetts General Hospital, Boston, MA; 3Massachusetts General Hospital, Harvard Medical School, Boston, MA; 4University of Milan, Vedano al Lambro, Lombardia, Italy; 5Humanitas university, Milan, Lombardia, Italy; 6Humanitas University, Milan, Lombardia, Italy; 7MGH, Brookline, MA
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1RA) are increasingly prescribed for diabetes management and weight loss. GLP-1RA decrease gastric motility, increasing the risk for adverse events in upper endoscopies (UE) due to higher risk of residual gastric content (RGC). This study evaluates the risks of GLP-1RA use during UE and sedation and assesses the impact of diabetes severity, GLP-1RA type, concomitant colonoscopy, and physical health status (ASA) on rates of RGC.
Methods: We identified index cases of patients on GLP-1RA at the time of UE from medical records from 2015-2024. Controls not on GLP-1RA were matched by age (± 5yrs), sex, race, diabetes status, BMI class, and ASA (1-4). Outcomes of interest included presence of RGC (volume and consistency blindly graded by 3 endoscopists), change in anesthesia plan, procedure termination, inability to reach duodenum, and aspiration events. We noted confounders for RGC (gastric surgeries, GI cancers, bowel obstruction) and compared the rates of RGC between cases and controls (Group A includes confounders, Group B excludes confounders). Among cases, we compared rates of RGC between GLP-1RA type, diabetes status and severity, ASA status, and concomitant colonoscopy.
Results: We identified 984 patients: mean age 60yrs, 63% female, 66% obese, and 74% type 2 diabetic. Group A had 581 cases and 403 controls; Group B had 440 cases and 321 controls. RGC rate was significantly higher in cases vs controls for both groups (p< 0.0001). There were no differences in RGC due to GLP-1RA type or diabetes status/severity. Among cases, patients with a low-risk ASA (1,2) and those with concomitant colonoscopy had significantly lower rates of RGC (p< 0.05). There were no complications from RGC in UE among controls. In cases, the rate of complications was low (< 1%). For those who experienced complications, most had a moderate/large amount and a semi-solid/solid consistency of RGC.
Discussion: GLP-1RA use is associated with significantly higher rates of RGC before and after accounting for confounders. Diabetes and type of GLP1-RA did not impact the rate of RGC, but patients having a concomitant colonoscopy and lower anesthetic risk had lower rates of RGC. Overall, GLP-1RA risks during UE are present but manageable with rare conversion to general anesthesia (GA) for safety and minor impact on completion of UE. Our results indicate that it may not be necessary to stop GLP-1RA for UE, but direct use of GA could mitigate complications in higher risk cases.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rebecca Karlson indicated no relevant financial relationships.
Jenna Clukey indicated no relevant financial relationships.
Victoria Beck indicated no relevant financial relationships.
Jonathan Kuang Ziyang indicated no relevant financial relationships.
Giulia Maria Corradini indicated no relevant financial relationships.
Mia Dekel indicated no relevant financial relationships.
Giulia Lojacono indicated no relevant financial relationships.
Akua Nuako indicated no relevant financial relationships.
Blythe Peterson indicated no relevant financial relationships.
Diane Somlo indicated no relevant financial relationships.
Nir Bar: Rafael pharmaceuticals – Grant/Research Support, Speakers Bureau. Sanofi – Grant/Research Support, Speakers Bureau.
Ion Hobai indicated no relevant financial relationships.
Braden Kuo: ATMO – Consultant, Grant/Research Support. Phathom – Consultant. Takeda – Advisory Committee/Board Member, Grant/Research Support.
Rebecca Karlson, BS1, Jenna Clukey, BA2, Victoria Beck, BA2, Jonathan Kuang Ziyang, MBBS3, Giulia Maria Corradini, MD4, Mia Dekel, 5, Giulia Lojacono, MS6, Akua Nuako, MD1, Blythe Peterson, BA1, Diane Somlo, MD, MBA1, Nir Bar, MD7, Ion Hobai, MD1, Braden Kuo, MD, MSc, FACG2. P0678 - Clinical Impact of GLP-1RA On Endoscopy: A Retrospective Cohort Study in Endoscopy Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
