Sunday Poster Session
Category: Esophagus
P0610 - From Dysphagia to Discovery: Unveiling a Mediastinal-Esophageal Fistula and Right Upper Lobe Abscess Post-Radiation Therapy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SR
Sahalia Rashid, MD, PhD
Wayne State University School of Medicine / Detroit Medical Center
Detroit, MI
Presenting Author(s)
Sahalia Rashid, MD, PhD1, Jasdeep Bathla, DO2, Komal Mendiratta, MD2, Katie Clark, 3, Emily Smith, 4, Mohammed Awad, MD1, Thomas Kelly, MD2
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Detroit Medical Center/Wayne State University, Detroit, MI; 3Wayne State University School of Medicine, Detroit, MI; 4Wayne State University, Detroit, MI
Introduction: Radiation therapy (RT) and chemotherapy are standard for advanced lung cancer but can lead to significant morbidity, including esophageal fistulas. Mediastinal-esophageal fistulas (MEF) are exceedingly rare, with an incidence of less than 1% of all esophageal fistulas. MEFs in the proximal esophagus are particularly uncommon, with tracheal-esophageal and bronchial-esophageal fistulas being more prevalent.
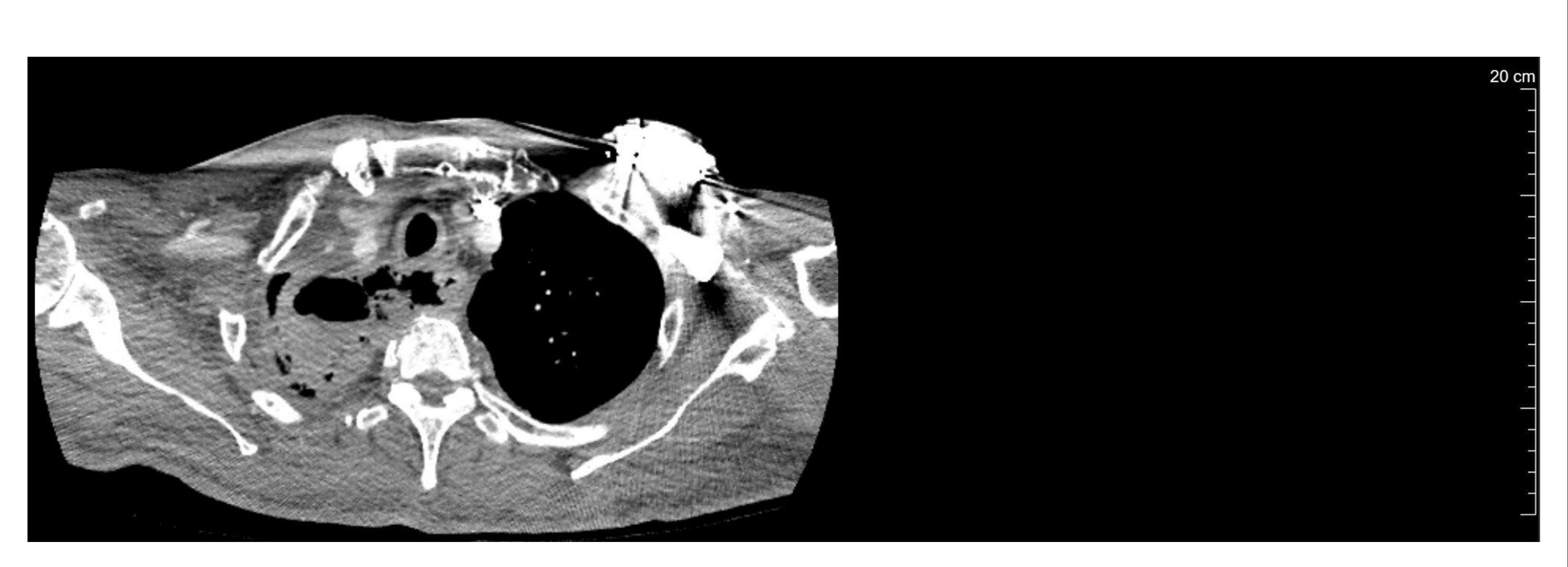
Case Description/Methods: A 77-year-old male with comorbidities including coronary artery disease, heart failure with reduced ejection fraction, diabetes mellitus, and stage IIIB squamous cell lung cancer (T4N2M0) diagnosed five months prior, presented with several months of dysphonia, dysphagia, odynophagia, epigastric abdominal pain, and emesis of solid food particles. He was vitally stable and afebrile upon presentation. The patient recently completed weekly chemotherapy with Carboplatin and Paclitaxel, radiation to the right lung, and was receiving adjuvant immunotherapy with Durvalumab. He had an exploratory esophagogastroduodenoscopy (EGD) just before admission, revealing a proximal esophageal defect filled with foamy white debris. He then underwent a computed tomography (CT) of the neck and thorax which revealed a mediastinal-esophageal necrotic fistula and a large air-fluid level mass in the right upper lobe (RUL). In conjunction with thoracic surgery, he was planned for bronchoscopy, repeat EGD for possible stent, and gastric tube placement. Chest x-ray showed new pneumonia surrounding the RUL abscess and sputum cultures revealed proteus mirabilis and pseudomonas aeruginosa, prompting initiation of cefepime, vancomycin and metronidazole. Unfortunately, the patient deteriorated clinically requiring ICU care and intubation, eventually developing multi-organ dysfunction resulting in his demise.
Discussion: This case highlights the interplay between comorbidities, malignancy, and the development of mediastinal-esophageal fistulas (MEF). MEFs are rare, but their clinical implications are profound, presenting diagnostic and therapeutic challenges. Management of such complex cases ranges from conservative methods like palliative care and nutritional support to invasive options such as endoscopic stenting and surgery. The optimal approach should involve multidisciplinary efforts and be individualized, considering the prognosis, fistula complexity, and tumor burden. Despite being an unfortunate complication, EFs warrant high clinical suspicion and early identification to prevent decompensation.
Disclosures:
Sahalia Rashid, MD, PhD1, Jasdeep Bathla, DO2, Komal Mendiratta, MD2, Katie Clark, 3, Emily Smith, 4, Mohammed Awad, MD1, Thomas Kelly, MD2. P0610 - From Dysphagia to Discovery: Unveiling a Mediastinal-Esophageal Fistula and Right Upper Lobe Abscess Post-Radiation Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Detroit Medical Center/Wayne State University, Detroit, MI; 3Wayne State University School of Medicine, Detroit, MI; 4Wayne State University, Detroit, MI
Introduction: Radiation therapy (RT) and chemotherapy are standard for advanced lung cancer but can lead to significant morbidity, including esophageal fistulas. Mediastinal-esophageal fistulas (MEF) are exceedingly rare, with an incidence of less than 1% of all esophageal fistulas. MEFs in the proximal esophagus are particularly uncommon, with tracheal-esophageal and bronchial-esophageal fistulas being more prevalent.
Case Description/Methods: A 77-year-old male with comorbidities including coronary artery disease, heart failure with reduced ejection fraction, diabetes mellitus, and stage IIIB squamous cell lung cancer (T4N2M0) diagnosed five months prior, presented with several months of dysphonia, dysphagia, odynophagia, epigastric abdominal pain, and emesis of solid food particles. He was vitally stable and afebrile upon presentation. The patient recently completed weekly chemotherapy with Carboplatin and Paclitaxel, radiation to the right lung, and was receiving adjuvant immunotherapy with Durvalumab. He had an exploratory esophagogastroduodenoscopy (EGD) just before admission, revealing a proximal esophageal defect filled with foamy white debris. He then underwent a computed tomography (CT) of the neck and thorax which revealed a mediastinal-esophageal necrotic fistula and a large air-fluid level mass in the right upper lobe (RUL). In conjunction with thoracic surgery, he was planned for bronchoscopy, repeat EGD for possible stent, and gastric tube placement. Chest x-ray showed new pneumonia surrounding the RUL abscess and sputum cultures revealed proteus mirabilis and pseudomonas aeruginosa, prompting initiation of cefepime, vancomycin and metronidazole. Unfortunately, the patient deteriorated clinically requiring ICU care and intubation, eventually developing multi-organ dysfunction resulting in his demise.
Discussion: This case highlights the interplay between comorbidities, malignancy, and the development of mediastinal-esophageal fistulas (MEF). MEFs are rare, but their clinical implications are profound, presenting diagnostic and therapeutic challenges. Management of such complex cases ranges from conservative methods like palliative care and nutritional support to invasive options such as endoscopic stenting and surgery. The optimal approach should involve multidisciplinary efforts and be individualized, considering the prognosis, fistula complexity, and tumor burden. Despite being an unfortunate complication, EFs warrant high clinical suspicion and early identification to prevent decompensation.
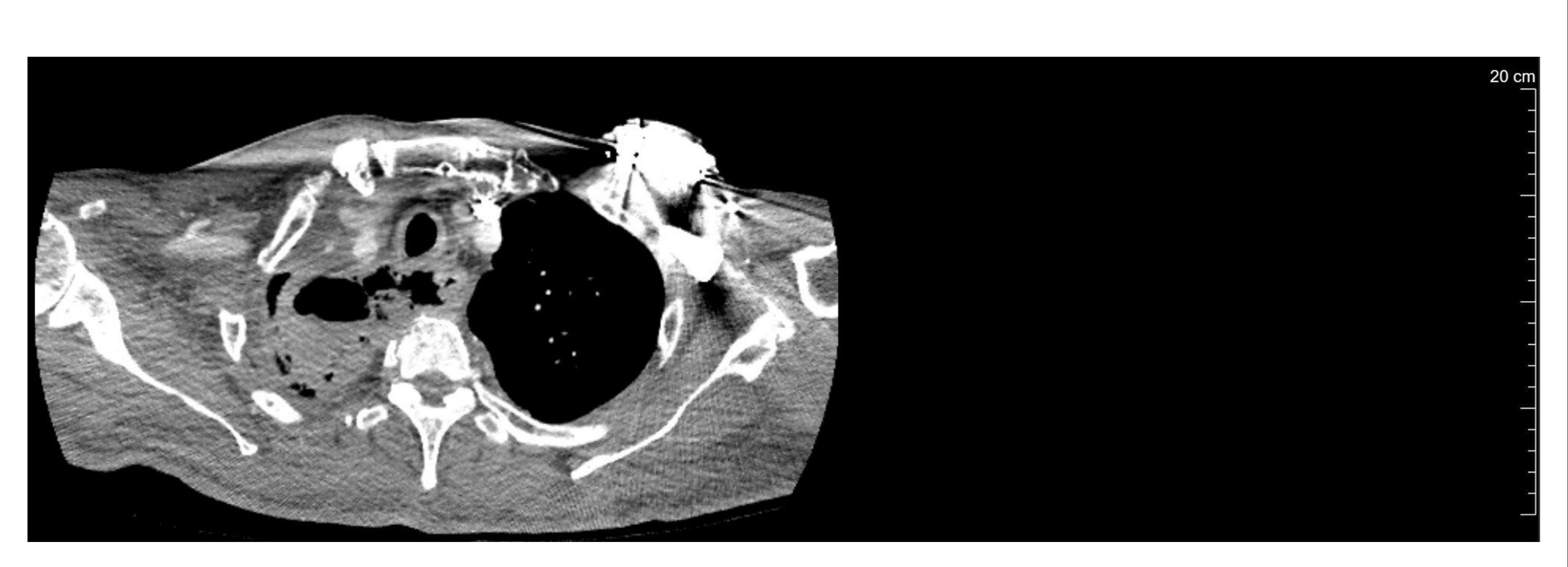
Figure: Fistula on CT Neck with contrast
Disclosures:
Sahalia Rashid indicated no relevant financial relationships.
Jasdeep Bathla indicated no relevant financial relationships.
Komal Mendiratta indicated no relevant financial relationships.
Katie Clark indicated no relevant financial relationships.
Emily Smith indicated no relevant financial relationships.
Mohammed Awad indicated no relevant financial relationships.
Thomas Kelly indicated no relevant financial relationships.
Sahalia Rashid, MD, PhD1, Jasdeep Bathla, DO2, Komal Mendiratta, MD2, Katie Clark, 3, Emily Smith, 4, Mohammed Awad, MD1, Thomas Kelly, MD2. P0610 - From Dysphagia to Discovery: Unveiling a Mediastinal-Esophageal Fistula and Right Upper Lobe Abscess Post-Radiation Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
