Sunday Poster Session
Category: Functional Bowel Disease
P0613 - Risk of Barrett’s Esophagus in Patients With Functional Dyspepsia: A Multi-Center Retrospective Cohort Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhammad Hassaan Arif Maan, MD
Rutgers New Jersey Medical School
Bloomfield, NJ
Presenting Author(s)
Muhammad Hassaan Arif Maan, MD1, Soban Maan, MD2, Imran A. Qureshi, MD3, Yazan Abboud, MD3, Wajiha Khan, MD4, Muhammad Mursaleen Ahmad, MBBS5, Muhammad Waleed, MD2
1Rutgers New Jersey Medical School, Bloomfield, NJ; 2West Virginia University, Morgantown, WV; 3Rutgers New Jersey Medical School, Newark, NJ; 4Rutgers New Jersey Medical School, Cartaret, NJ; 5Punjab Institute of Medical Sciences, Bloomfield, NJ
Introduction: Dyspepsia refers to a set of gastroduodenal symptoms such as epigastric pain or burning, postprandial fullness, or early satiety. Most dyspepsia cases do not have an underlying structural explanation for the symptoms and are attributed to functional dyspepsia (FD). Whereas evidence of gastritis on endoscopy and its association with esophageal dysplasia is well-studied, data about the association between FD and the risk of developing esophageal metaplasia/dysplasia is scarce.
Methods: We performed a multi-center cohort study using an electronic health records-based research network, TriNetX to assess the association of FD and Barrett’s Esophagus (BE). 1:1 propensity score matching was used to match patients with the diagnosis of FD between January 1, 2006, and December 31, 2022, with those without FD diagnosis (control) to minimize confounding. Patients who had diagnoses of BE or esophageal cancer before the study period were excluded. Both groups were matched for age, gender, race, ethnicity, elevated body mass index, smoking, alcohol use, gastroesophageal reflux disease (GERD), and proton pump inhibitor (PPI) use at baseline. We used the diagnosis of BE as our primary outcome. Hazard ratios (HRs) with their corresponding 95% confidence intervals were calculated. As GERD and BE can be silent and may remain undetected, we employed sensitivity analysis to specifically compare outcomes in patients who had undergone esophagogastroduodenoscopy (EGD) after being included in the study.
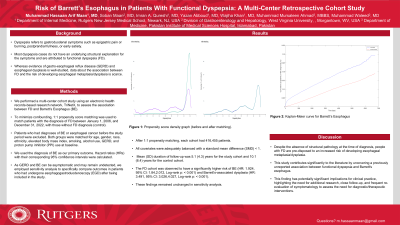
Results: After 1:1 propensity matching, each cohort had 416,455 patients. The cohorts were adequately balanced with a standard mean difference (SMD) ≤ 0.1 for all selected covariates (Table 1). Mean (SD) duration of follow-up was 5.1 (4.3) years for the study cohort and 10.1 (6.4) years for the control cohort. The FD cohort was observed to have a significantly higher risk of BE (HR: 1.924, 95% CI: 1.84,2.012, Log-rank p: < 0.001) and Barrett’s-associated dysplasia (HR: 3.491, 95% CI: 3.026,4.027, Log-rank p: < 0.001). These findings remained unchanged in sensitivity analysis.
Discussion: Despite the absence of structural pathology at the time of diagnosis, people with functional dyspepsia are pre-disposed to an increased risk of developing esophageal metaplasia/dysplasia. This warrants close follow-up and frequent re-evaluation of symptomatology to assess the need for diagnostic/therapeutic interventions.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Muhammad Hassaan Arif Maan, MD1, Soban Maan, MD2, Imran A. Qureshi, MD3, Yazan Abboud, MD3, Wajiha Khan, MD4, Muhammad Mursaleen Ahmad, MBBS5, Muhammad Waleed, MD2. P0613 - Risk of Barrett’s Esophagus in Patients With Functional Dyspepsia: A Multi-Center Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Bloomfield, NJ; 2West Virginia University, Morgantown, WV; 3Rutgers New Jersey Medical School, Newark, NJ; 4Rutgers New Jersey Medical School, Cartaret, NJ; 5Punjab Institute of Medical Sciences, Bloomfield, NJ
Introduction: Dyspepsia refers to a set of gastroduodenal symptoms such as epigastric pain or burning, postprandial fullness, or early satiety. Most dyspepsia cases do not have an underlying structural explanation for the symptoms and are attributed to functional dyspepsia (FD). Whereas evidence of gastritis on endoscopy and its association with esophageal dysplasia is well-studied, data about the association between FD and the risk of developing esophageal metaplasia/dysplasia is scarce.
Methods: We performed a multi-center cohort study using an electronic health records-based research network, TriNetX to assess the association of FD and Barrett’s Esophagus (BE). 1:1 propensity score matching was used to match patients with the diagnosis of FD between January 1, 2006, and December 31, 2022, with those without FD diagnosis (control) to minimize confounding. Patients who had diagnoses of BE or esophageal cancer before the study period were excluded. Both groups were matched for age, gender, race, ethnicity, elevated body mass index, smoking, alcohol use, gastroesophageal reflux disease (GERD), and proton pump inhibitor (PPI) use at baseline. We used the diagnosis of BE as our primary outcome. Hazard ratios (HRs) with their corresponding 95% confidence intervals were calculated. As GERD and BE can be silent and may remain undetected, we employed sensitivity analysis to specifically compare outcomes in patients who had undergone esophagogastroduodenoscopy (EGD) after being included in the study.
Results: After 1:1 propensity matching, each cohort had 416,455 patients. The cohorts were adequately balanced with a standard mean difference (SMD) ≤ 0.1 for all selected covariates (Table 1). Mean (SD) duration of follow-up was 5.1 (4.3) years for the study cohort and 10.1 (6.4) years for the control cohort. The FD cohort was observed to have a significantly higher risk of BE (HR: 1.924, 95% CI: 1.84,2.012, Log-rank p: < 0.001) and Barrett’s-associated dysplasia (HR: 3.491, 95% CI: 3.026,4.027, Log-rank p: < 0.001). These findings remained unchanged in sensitivity analysis.
Discussion: Despite the absence of structural pathology at the time of diagnosis, people with functional dyspepsia are pre-disposed to an increased risk of developing esophageal metaplasia/dysplasia. This warrants close follow-up and frequent re-evaluation of symptomatology to assess the need for diagnostic/therapeutic interventions.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Muhammad Hassaan Arif Maan indicated no relevant financial relationships.
Soban Maan indicated no relevant financial relationships.
Imran Qureshi indicated no relevant financial relationships.
Yazan Abboud indicated no relevant financial relationships.
Wajiha Khan indicated no relevant financial relationships.
Muhammad Mursaleen Ahmad indicated no relevant financial relationships.
Muhammad Waleed indicated no relevant financial relationships.
Muhammad Hassaan Arif Maan, MD1, Soban Maan, MD2, Imran A. Qureshi, MD3, Yazan Abboud, MD3, Wajiha Khan, MD4, Muhammad Mursaleen Ahmad, MBBS5, Muhammad Waleed, MD2. P0613 - Risk of Barrett’s Esophagus in Patients With Functional Dyspepsia: A Multi-Center Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
