Sunday Poster Session
Category: Esophagus
P0545 - Esophageal Management of an Aortoesophageal Fistula
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- RG
Robert S. Gordon, III, MS, DO
George Washington University School of Medicine and Health Sciences
Alexandria, VA
Presenting Author(s)
Robert S. Gordon, MS, DO, Zahra Al Monsoori, MD, Samuel A.. Schueler, MD, Marie L.. Borum, MD, MPH, FACG
George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Aortoesophageal fistula (AEF) carries a 100% mortality rate if untreated. Given the low incidence, standard management remains unclear. Strategies include thoracic endovascular aortic repair (TEVAR) and/or graft replacement for management of the aorta and stenting or esophagectomy for the esophagus. This case highlights the need for further studies to establish standardized management of AEFs.
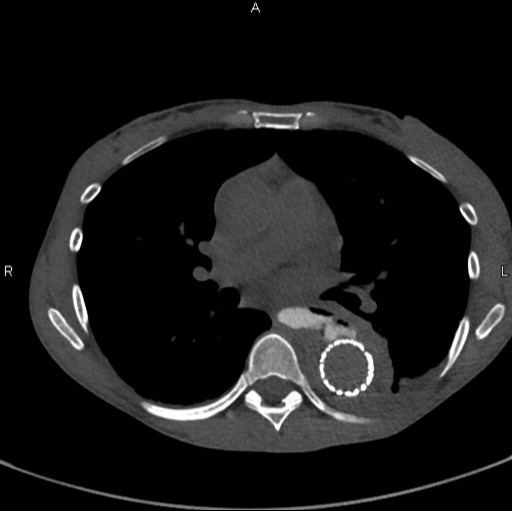
Case Description/Methods: A 49-year-old female with hypertension, atrial fibrillation, cryptogenic infarcts, and cyclic vomiting presented with hypertensive emergency with two days of chest pain radiating to her back. A computed tomography angiogram (CTA) chest demonstrated a type B aortic dissection. Anti-impulse therapy was initiated and the patient underwent TEVAR. The post-procedural course was complicated by severe back pain, ileus, and hematochezia requiring multiple blood transfusions. CTA findings were concerning for a fistula between the esophagus and the false lumen of the aorta, confirmed via CT esophagram (Figure 1). Esophagogastroduodenoscopy (EGD) was notable for a large esophageal perforation through which the aortic stent was visible. A fully-covered metal esophageal stent was deployed across the perforation. A subsequent CTA chest with oral contrast demonstrated a continued leak of oral contrast into the aortic false lumen. The original stent was removed and replaced by two overlapping fully-covered metal esophageal stents. An Esophagram showed continued contrast leak, resulting in esophageal stent removal, cervical esophagostomy, and placement of a gastrojejunostomy tube. The patient returned within 24 hours of discharge in hypertensive emergency with a new aortic dissection. The patient passed away several days later due to related complications.
Discussion: AEF is a rare, life-threatening condition without well-defined standard of treatment. Our patient was initially managed with two attempts of esophageal stenting before requiring esophagostomy. While esophageal stenting presents a less invasive management strategy, an early surgical approach may reduce the risk of severe hemorrhage and sepsis. Further studies are required to compare relative efficacy of esophageal stenting versus surgical management in the setting of AEF.
Disclosures:
Robert S. Gordon, MS, DO, Zahra Al Monsoori, MD, Samuel A.. Schueler, MD, Marie L.. Borum, MD, MPH, FACG. P0545 - Esophageal Management of an Aortoesophageal Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
George Washington University School of Medicine and Health Sciences, Washington, DC
Introduction: Aortoesophageal fistula (AEF) carries a 100% mortality rate if untreated. Given the low incidence, standard management remains unclear. Strategies include thoracic endovascular aortic repair (TEVAR) and/or graft replacement for management of the aorta and stenting or esophagectomy for the esophagus. This case highlights the need for further studies to establish standardized management of AEFs.
Case Description/Methods: A 49-year-old female with hypertension, atrial fibrillation, cryptogenic infarcts, and cyclic vomiting presented with hypertensive emergency with two days of chest pain radiating to her back. A computed tomography angiogram (CTA) chest demonstrated a type B aortic dissection. Anti-impulse therapy was initiated and the patient underwent TEVAR. The post-procedural course was complicated by severe back pain, ileus, and hematochezia requiring multiple blood transfusions. CTA findings were concerning for a fistula between the esophagus and the false lumen of the aorta, confirmed via CT esophagram (Figure 1). Esophagogastroduodenoscopy (EGD) was notable for a large esophageal perforation through which the aortic stent was visible. A fully-covered metal esophageal stent was deployed across the perforation. A subsequent CTA chest with oral contrast demonstrated a continued leak of oral contrast into the aortic false lumen. The original stent was removed and replaced by two overlapping fully-covered metal esophageal stents. An Esophagram showed continued contrast leak, resulting in esophageal stent removal, cervical esophagostomy, and placement of a gastrojejunostomy tube. The patient returned within 24 hours of discharge in hypertensive emergency with a new aortic dissection. The patient passed away several days later due to related complications.
Discussion: AEF is a rare, life-threatening condition without well-defined standard of treatment. Our patient was initially managed with two attempts of esophageal stenting before requiring esophagostomy. While esophageal stenting presents a less invasive management strategy, an early surgical approach may reduce the risk of severe hemorrhage and sepsis. Further studies are required to compare relative efficacy of esophageal stenting versus surgical management in the setting of AEF.
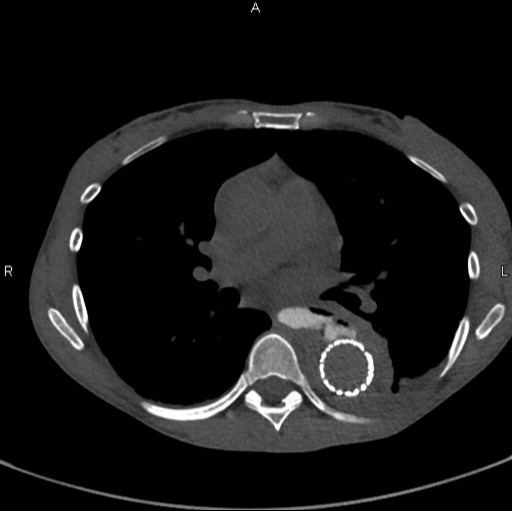
Figure: Figure 1. Computed Tomography Esophagram, axial plane, oral contrast observed within the false lumen of the thoracic aorta status post thoracic endovascular aortic repair, indicative of a fistulous connection between the esophagus and the aorta.
Disclosures:
Robert Gordon indicated no relevant financial relationships.
Zahra Al Monsoori indicated no relevant financial relationships.
Samuel Schueler indicated no relevant financial relationships.
Marie Borum: Takeda Pharmaceuticals – Consultant, Speakers Bureau.
Robert S. Gordon, MS, DO, Zahra Al Monsoori, MD, Samuel A.. Schueler, MD, Marie L.. Borum, MD, MPH, FACG. P0545 - Esophageal Management of an Aortoesophageal Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
