Sunday Poster Session
Category: Esophagus
P0547 - Peripartum Respiratory Distress: A Breathtaking Initial Presentation of Achalasia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Harrison Pajovich, MD
Lankenau Medical Center
Philadelphia, PA
Presenting Author(s)
Harrison Pajovich, MD1, Stefanie Gallagher, DO2, Amanda Long, DO2, Adam Kaufman, MD2
1Lankenau Medical Center, Philadelphia, PA; 2Lankenau Medical Center, Wynnewood, PA
Introduction: Achalasia in pregnancy is a rare clinical entity and can, initially, be misdiagnosed as GERD or hyperemesis gravidarum. Identifying and addressing achalasia during pregnancy becomes imperative due to its potential for severe consequences, including malnutrition, preterm birth, and fetal growth restriction or demise. Prompt diagnosis and intervention are essential despite the scarcity of definitive guidelines. We present a case of respiratory distress, due to airway compromise from a large food bolus due to underlying, newly diagnosed achalasia.
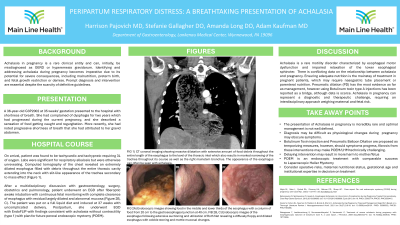
Case Description/Methods: A 36-year-old G3P2002 at 35 weeks gestation presented with acute-onset respiratory distress, and found to be tachycardic and tachypneic, requiring 3L of oxygen. CT chest revealed an extremely dilated esophagus filled with debris throughout the entire thoracic cavity extending into the neck with slit-like appearance of the trachea secondary to mass effect (Figure 1). The patient complained of dysphagia for 2 years, which progressively worsened during her current pregnancy with symptoms of food getting caught and regurgitation. She also noted progressive shortness of breath that she attributed to her gravid abdomen. After a multidisciplinary discussion with gastroenterology, surgery, obstetrics and pulmonology, patient underwent an EGD after fiberoptic awake intubation with continuous fetal monitoring with complete clearance of esophagus with residual largely dilated and abnormal mucosa (Figure 2B, C). The patient was put on a full liquid diet and induced at 37 weeks with uncomplicated delivery. Postpartum, she underwent EGD with EndoFLIP with findings consistent with achalasia without contractility (type 1) with plan for future peroral endoscopic myotomy (POEM).
Discussion: Achalasia is a rare motility disorder characterized by esophageal motor dysfunction and impaired relaxation of the lower esophageal sphincter. There is conflicting data on the relationship between achalasia and pregnancy. Ensuring adequate nutrition is the mainstay of treatment in pregnant patients, which may require nasogastric tube placement or parenteral nutrition. Pneumatic dilation (PD) has the most evidence as far as management, however using Botulinum toxin type A injections has been reported as a bridge, although data is scarce. Achalasia in pregnancy can represent a diagnostic and therapeutic challenge, requiring an interdisciplinary approach weighing maternal and fetal risk.
Disclosures:
Harrison Pajovich, MD1, Stefanie Gallagher, DO2, Amanda Long, DO2, Adam Kaufman, MD2. P0547 - Peripartum Respiratory Distress: A Breathtaking Initial Presentation of Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lankenau Medical Center, Philadelphia, PA; 2Lankenau Medical Center, Wynnewood, PA
Introduction: Achalasia in pregnancy is a rare clinical entity and can, initially, be misdiagnosed as GERD or hyperemesis gravidarum. Identifying and addressing achalasia during pregnancy becomes imperative due to its potential for severe consequences, including malnutrition, preterm birth, and fetal growth restriction or demise. Prompt diagnosis and intervention are essential despite the scarcity of definitive guidelines. We present a case of respiratory distress, due to airway compromise from a large food bolus due to underlying, newly diagnosed achalasia.
Case Description/Methods: A 36-year-old G3P2002 at 35 weeks gestation presented with acute-onset respiratory distress, and found to be tachycardic and tachypneic, requiring 3L of oxygen. CT chest revealed an extremely dilated esophagus filled with debris throughout the entire thoracic cavity extending into the neck with slit-like appearance of the trachea secondary to mass effect (Figure 1). The patient complained of dysphagia for 2 years, which progressively worsened during her current pregnancy with symptoms of food getting caught and regurgitation. She also noted progressive shortness of breath that she attributed to her gravid abdomen. After a multidisciplinary discussion with gastroenterology, surgery, obstetrics and pulmonology, patient underwent an EGD after fiberoptic awake intubation with continuous fetal monitoring with complete clearance of esophagus with residual largely dilated and abnormal mucosa (Figure 2B, C). The patient was put on a full liquid diet and induced at 37 weeks with uncomplicated delivery. Postpartum, she underwent EGD with EndoFLIP with findings consistent with achalasia without contractility (type 1) with plan for future peroral endoscopic myotomy (POEM).
Discussion: Achalasia is a rare motility disorder characterized by esophageal motor dysfunction and impaired relaxation of the lower esophageal sphincter. There is conflicting data on the relationship between achalasia and pregnancy. Ensuring adequate nutrition is the mainstay of treatment in pregnant patients, which may require nasogastric tube placement or parenteral nutrition. Pneumatic dilation (PD) has the most evidence as far as management, however using Botulinum toxin type A injections has been reported as a bridge, although data is scarce. Achalasia in pregnancy can represent a diagnostic and therapeutic challenge, requiring an interdisciplinary approach weighing maternal and fetal risk.
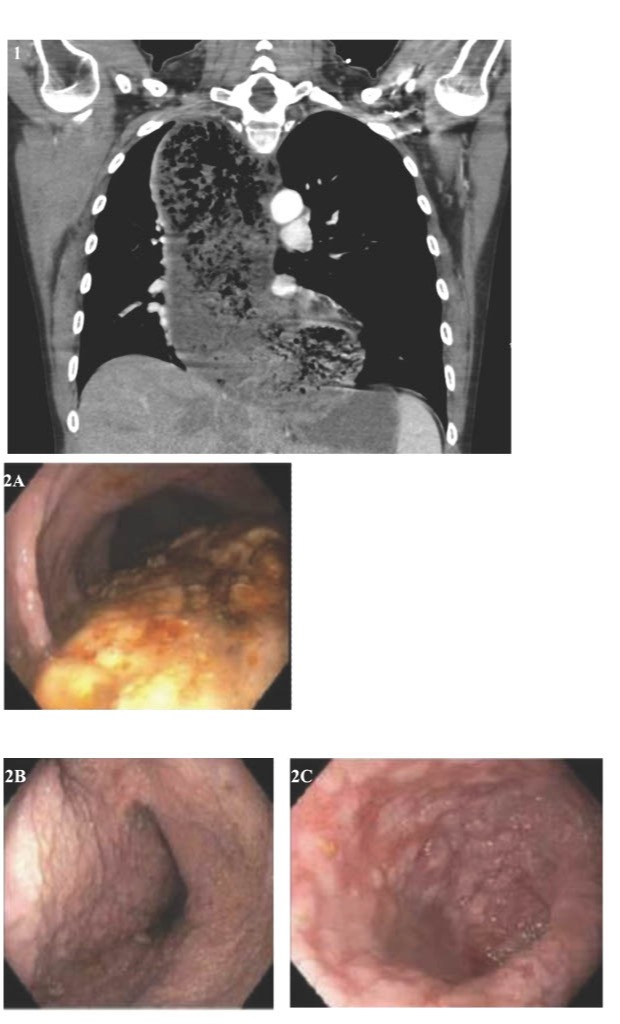
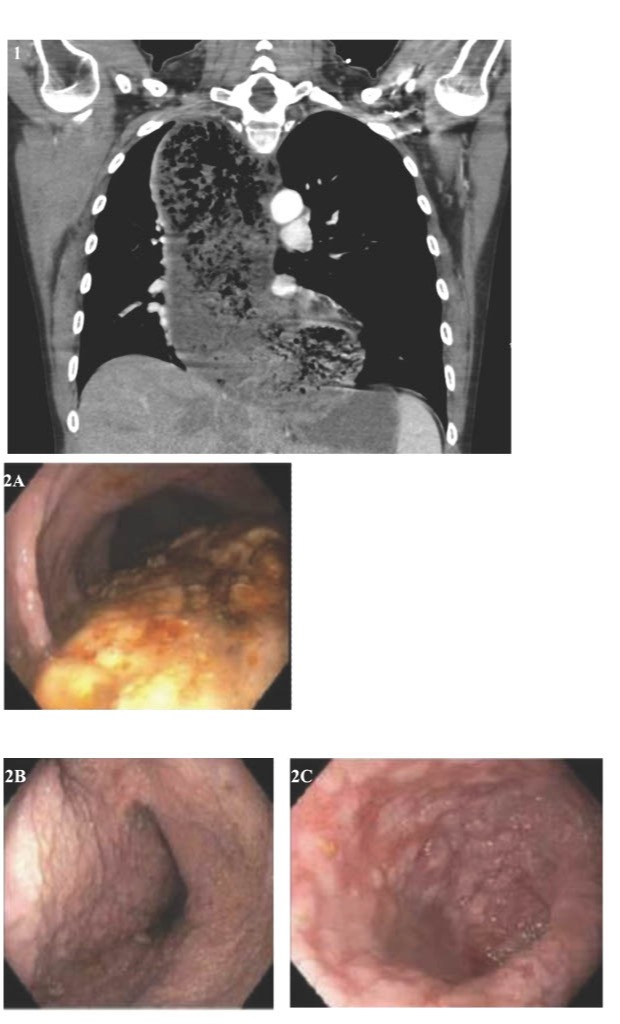
Figure: FIGURE 1: CT coronal imaging showing massive dilatation with extensive amount of food debris throughout the entire length of the esophagus to the level of the thoracic inlet which also results in marked narrowing of the trachea throughout its course as well as the right mainstem bronchus. The appearance of the esophagus can often be seen with achalasia. FIGURE 2A: Endoscopic images showing food in the middle and lower thirds of the esophagus with column of food from 20 cm to the gastroesophageal junction at 40 cm.
FIGURE 2B, C: Endoscopic images of the esophagus following extensive suction and utilization of Roth net revealing a diffusely floppy and dilater esophagus with cobble stoning and mottle mucosal changes.
FIGURE 2B, C: Endoscopic images of the esophagus following extensive suction and utilization of Roth net revealing a diffusely floppy and dilater esophagus with cobble stoning and mottle mucosal changes.
Disclosures:
Harrison Pajovich indicated no relevant financial relationships.
Stefanie Gallagher indicated no relevant financial relationships.
Amanda Long indicated no relevant financial relationships.
Adam Kaufman indicated no relevant financial relationships.
Harrison Pajovich, MD1, Stefanie Gallagher, DO2, Amanda Long, DO2, Adam Kaufman, MD2. P0547 - Peripartum Respiratory Distress: A Breathtaking Initial Presentation of Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
