Sunday Poster Session
Category: Esophagus
P0562 - A Case of Plummer Vinson Syndrome in Cirrhosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Daniella Mikhail, MD
Robert Wood Johnson Medical School, Rutgers University
North Brunswick Township, NJ
Presenting Author(s)
Daniella Mikhail, MD1, Toni Marie Chandler, MD2, Anish V. Patel, MD2
1Robert Wood Johnson Medical School, Rutgers University, North Brunswick Township, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Plummer Vinson Syndrome (PVS) is defined as triad of dysphagia, iron-deficiency anemia (IDA), and esophageal webbing. It is an uncommon etiology of dysphagia. The exact etiology of this syndrome is unknown, however iron deficiency may be playing a role at the formation of the esophageal webs.
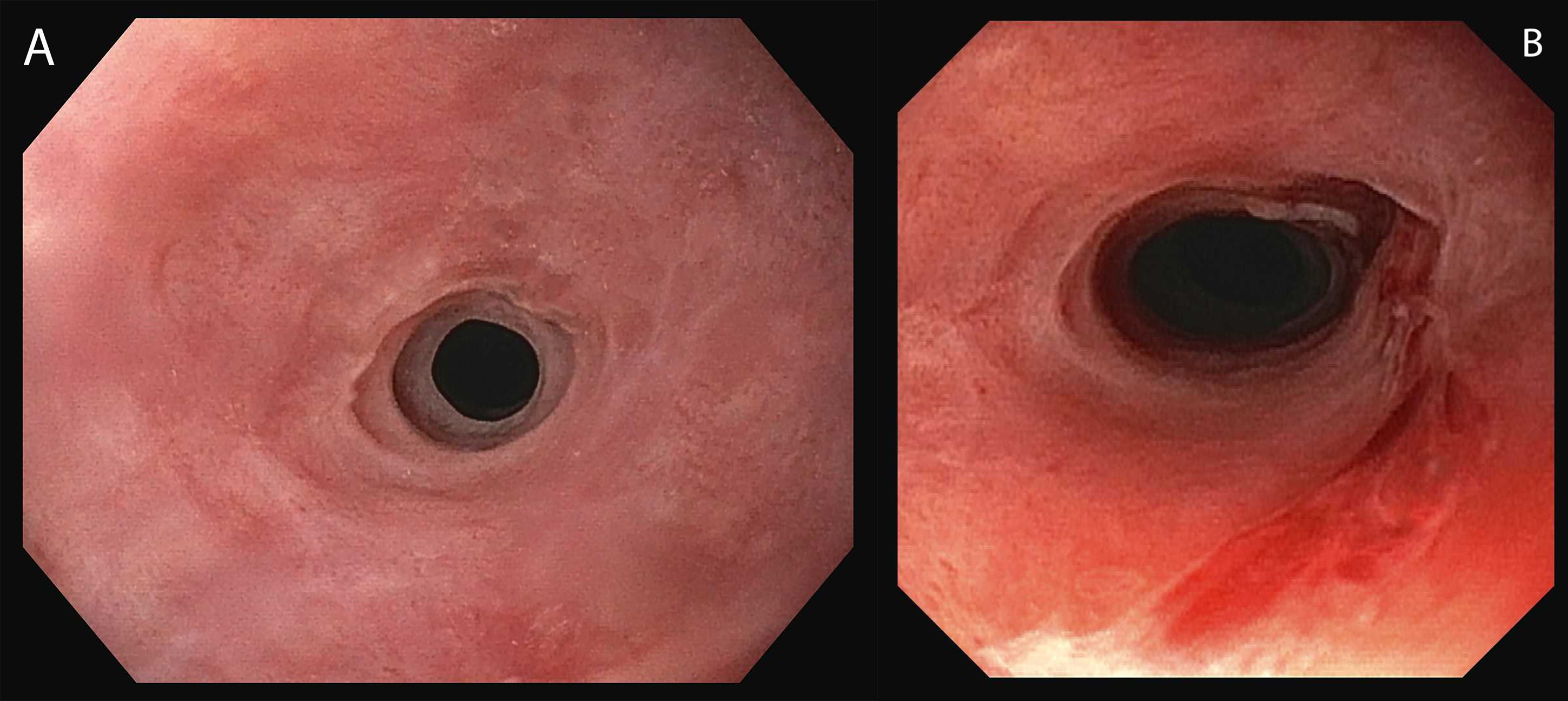
Case Description/Methods: 58 year-old Hispanic male with newly diagnosed NASH cirrhosis presented with dysphagia and associated 20–30-pound weight loss over several weeks. Initial laboratory evaluation showed microcytic anemia with hemoglobin 7.1 g/dL. Workup of anemia revealed total iron saturation 11%, ferritin 42 ng/mL, iron 17 mcg/dL. He denied overt GI bleeding. Upper endoscopy was performed, which revealed 2 benign appearing strictures in the proximal esophagus (Figure 1A). These strictures were 5mm in diameter, at 20 and 22cm from the incisors, and only traversable by downsizing the endoscope. Esophageal biopsies revealed normal squamous mucosa but no intestinal metaplasia, dysplasia, or eosinophils. The constellation of dysphagia, IDA, upper esophageal strictures, and normal esophageal biopsy fit the diagnosis of PVS. Patient underwent an additional endoscopy with balloon dilation of both strictures to 8mm (Figure 1B). He was discharged on pureed diet and scheduled for repeat endoscopy in 1 month. His IDA was treated with intravenous and then oral iron supplementation. Patient did undergo repeat endoscopy 1 month later during a subsequent hospitalization for decompensated cirrhosis. Endoscopy re-demonstrated the severe strictures at 20cm and 22cm, both of which were balloon dilated to 8mm. Patient’s overall clinical course declined after having a spontaneous intracranial hemorrhage and expired during this hospitalization.
Discussion: PVS should be suspected when proximal esophageal webs or strictures are identified. It is important to take esophageal biopsies to rule out other etiologies of dysphagia such as eosinophilic esophagitis, malignancy, pemphigus vulgaris, lichen planus and chronic reflux. There has been some evidence of improved dysphagia symptoms with iron supplementation. In patients with significant strictures seen on endoscopy, such as in our patient, dilation may be required. PVS has been associated with esophageal or pharyngeal squamous cell carcinoma, therefore identifying this syndrome holds clinical significance. Annual surveillance endoscopy should be considered. To our knowledge, our patient is one of the rare cases of PVS reported with underlying cirrhosis.
Disclosures:
Daniella Mikhail, MD1, Toni Marie Chandler, MD2, Anish V. Patel, MD2. P0562 - A Case of Plummer Vinson Syndrome in Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Robert Wood Johnson Medical School, Rutgers University, North Brunswick Township, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Plummer Vinson Syndrome (PVS) is defined as triad of dysphagia, iron-deficiency anemia (IDA), and esophageal webbing. It is an uncommon etiology of dysphagia. The exact etiology of this syndrome is unknown, however iron deficiency may be playing a role at the formation of the esophageal webs.
Case Description/Methods: 58 year-old Hispanic male with newly diagnosed NASH cirrhosis presented with dysphagia and associated 20–30-pound weight loss over several weeks. Initial laboratory evaluation showed microcytic anemia with hemoglobin 7.1 g/dL. Workup of anemia revealed total iron saturation 11%, ferritin 42 ng/mL, iron 17 mcg/dL. He denied overt GI bleeding. Upper endoscopy was performed, which revealed 2 benign appearing strictures in the proximal esophagus (Figure 1A). These strictures were 5mm in diameter, at 20 and 22cm from the incisors, and only traversable by downsizing the endoscope. Esophageal biopsies revealed normal squamous mucosa but no intestinal metaplasia, dysplasia, or eosinophils. The constellation of dysphagia, IDA, upper esophageal strictures, and normal esophageal biopsy fit the diagnosis of PVS. Patient underwent an additional endoscopy with balloon dilation of both strictures to 8mm (Figure 1B). He was discharged on pureed diet and scheduled for repeat endoscopy in 1 month. His IDA was treated with intravenous and then oral iron supplementation. Patient did undergo repeat endoscopy 1 month later during a subsequent hospitalization for decompensated cirrhosis. Endoscopy re-demonstrated the severe strictures at 20cm and 22cm, both of which were balloon dilated to 8mm. Patient’s overall clinical course declined after having a spontaneous intracranial hemorrhage and expired during this hospitalization.
Discussion: PVS should be suspected when proximal esophageal webs or strictures are identified. It is important to take esophageal biopsies to rule out other etiologies of dysphagia such as eosinophilic esophagitis, malignancy, pemphigus vulgaris, lichen planus and chronic reflux. There has been some evidence of improved dysphagia symptoms with iron supplementation. In patients with significant strictures seen on endoscopy, such as in our patient, dilation may be required. PVS has been associated with esophageal or pharyngeal squamous cell carcinoma, therefore identifying this syndrome holds clinical significance. Annual surveillance endoscopy should be considered. To our knowledge, our patient is one of the rare cases of PVS reported with underlying cirrhosis.
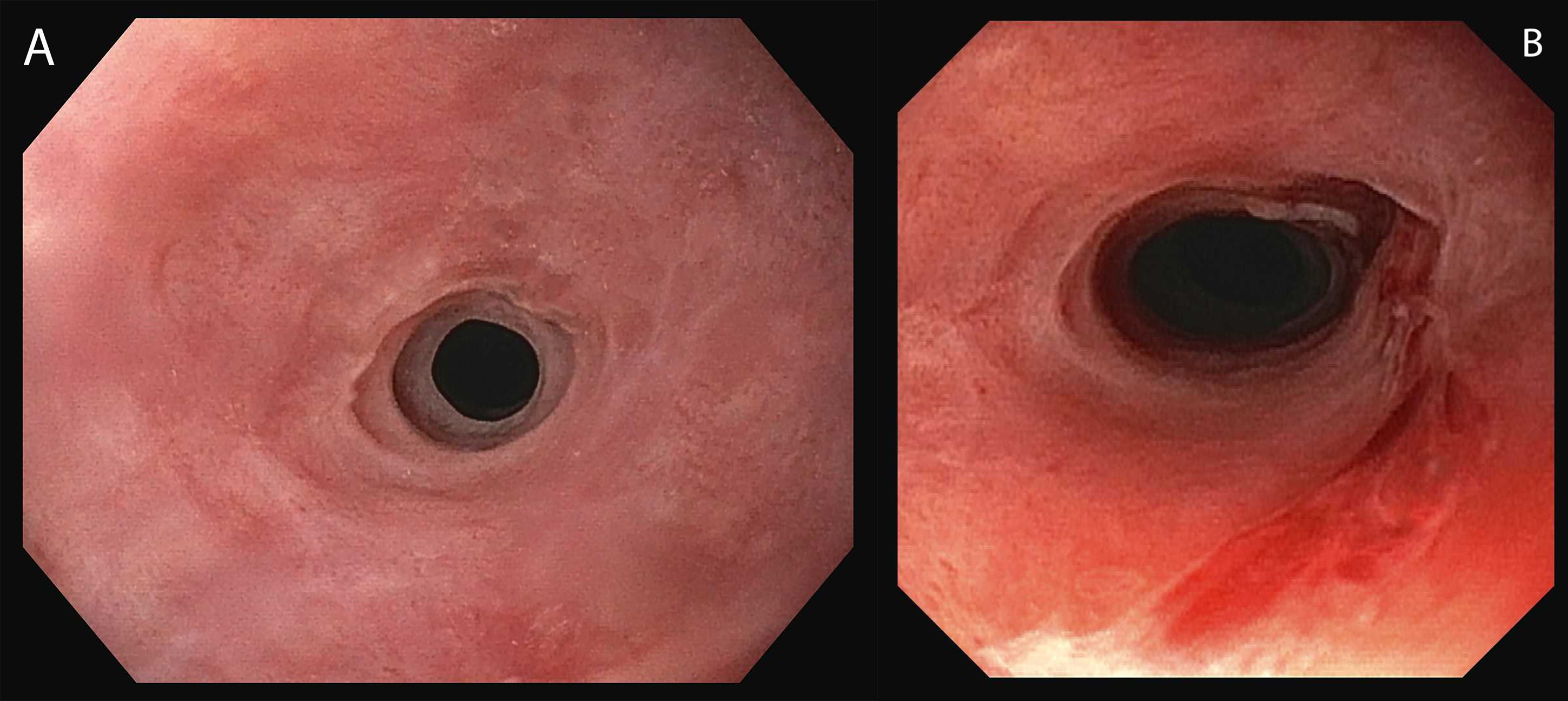
Figure: A. Initial esophagogastroduodenoscopy (EGD) revealing 2 benign appearing strictures in the proximal esophagus.
B. Subsequent EGD after undergoing balloon dilation of both stricutres.
B. Subsequent EGD after undergoing balloon dilation of both stricutres.
Disclosures:
Daniella Mikhail indicated no relevant financial relationships.
Toni Marie Chandler indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Daniella Mikhail, MD1, Toni Marie Chandler, MD2, Anish V. Patel, MD2. P0562 - A Case of Plummer Vinson Syndrome in Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
