Sunday Poster Session
Category: Esophagus
P0469 - Chicago Classification Version 4.0 Manometric Diagnoses in Surgery-Naïve Obese Patients and Obese Patients After Bariatric Surgery
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ambreen A. Merchant, MD
Baylor University Medical Center
Farmer Branch, TX
Presenting Author(s)
Ambreen Anil Merchant, MD1, Anjali Bhatt, BS2, Daisha J.. Cipher, PhD3, Ashton Ellison, MBBCh4, Chanakyaram A.. Reddy, MD5, Daniel Davis, DO6, Rhonda F.. Souza, MD7, Vani J.A.. Konda, MD4, Stuart J.. Spechler, MD4, Anh D.. Nguyen, MD4
1Baylor University Medical Center, Farmer Branch, TX; 2Texas A&M School of Medicine, Sugar Land, TX; 3University of Texas, Arlington, TX; 4Baylor University Medical Center and Center for Esophageal Research, Baylor Scott & White Research Institute, Dallas, TX; 5Center for Esophageal Diseases, Baylor Scott & White Medical Center, Dallas, TX; 6Baylor Scott & White Center for Medical & Surgical Weight Loss Management, Dallas, TX; 7Baylor Scott & White Research Institute, Dallas, TX
Introduction: Several studies predating publication of Chicago Classification v4.0 (CCv4.0) found that high resolution manometry (HRM) often revealed motility disorders in obese patients who had bariatric surgery, but few data are available on HRM findings interpreted by CCv4.0 in obese patients. The primary aims of this study were to compare CCv4.0 motility diagnoses in obese patients undergoing evaluation for initial bariatric surgery with those who had undergone bariatric surgery, and to identify differences in CCv4.0 diagnoses among patients who had different types of bariatric surgery.
Methods: We analyzed our clinical database from April 2019 to March 2023 to identify obese patients who had HRM during evaluation for initial bariatric surgery (surgery-naïve group) or during evaluation after prior sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), or laparoscopic gastric band (LGB) surgery that resulted in insufficient weight loss (“postsurgical group”). Patients who had other foregut surgery besides SG, RYGB or LGB were excluded.
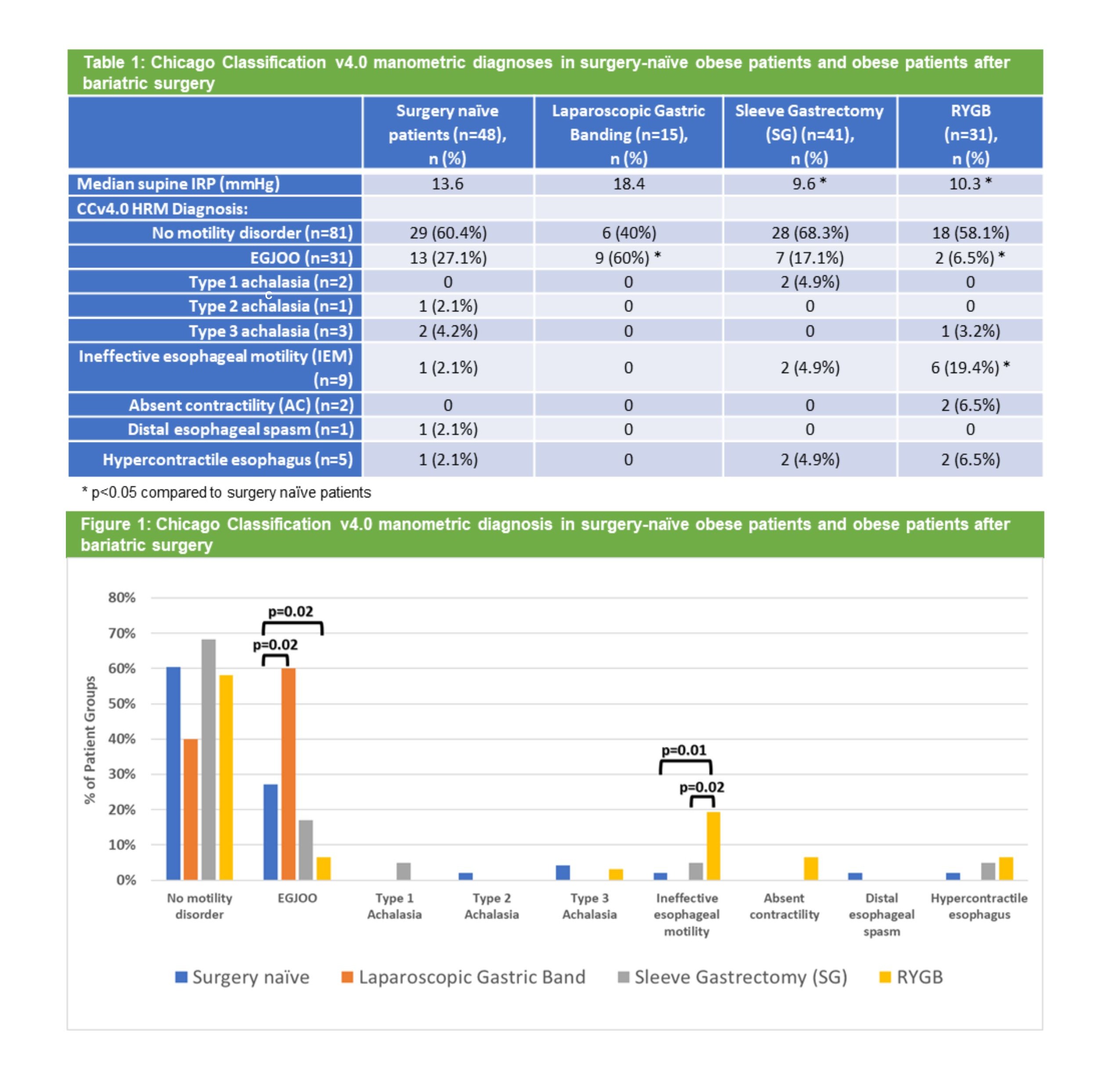
Results: We identified 48 surgery-naïve and 87 postsurgical patients (41 SG, 31 RYGB, 15 LGB). Presenting symptoms were: 58% dysphagia, 44% heartburn, 27% chest pain, 21% regurgitation, 7% other (abdominal pain, bloating, or nausea), 9% no symptoms. Compared to surgery-naïve patients, the median supine integrated relaxation pressure (IRP) was lower in SG (9.6 vs 13.6 mmHg, p=0.04) and RYGB patients (10.3 vs 13.6 mmHg, p=0.02), and higher in LGB patients (18.4 vs 13.6 mmHg, p=0.41) (Table 1). CCv4.0 manometric diagnoses were common across all four groups (Figure 1), particularly in LGB patients. Esophagogastric junction outflow obstruction (EGJOO) was the most frequent manometric diagnosis in surgery-naïve (27.1%), SG (17.1%), and LGB patients (60%), but was infrequent in RYGB patients (6.5%). Conversely, ineffective esophageal motility (IEM) was common in RYGB patients (19.4%) but rare in surgery-naïve (2.1%), SG (4.9%), and LGB (0%) patients. Compared to the surgery-naïve group, EGJOO was less frequent (p=0.02) and IEM was more frequent (p=0.01) in the RYGB patients.
Discussion: Esophageal motility disorders by CCv4.0 are common in obese patients, both before and after bariatric surgery. EGJOO is frequent in surgery-naïve, SG and LGB patients, but not in RYGB patients. Conversely, RYGB patients exhibit a higher frequency of IEM compared to the other groups. Further studies are needed to assess the clinical significance of these frequent manometric abnormalities.
Disclosures:
Ambreen Anil Merchant, MD1, Anjali Bhatt, BS2, Daisha J.. Cipher, PhD3, Ashton Ellison, MBBCh4, Chanakyaram A.. Reddy, MD5, Daniel Davis, DO6, Rhonda F.. Souza, MD7, Vani J.A.. Konda, MD4, Stuart J.. Spechler, MD4, Anh D.. Nguyen, MD4. P0469 - Chicago Classification Version 4.0 Manometric Diagnoses in Surgery-Naïve Obese Patients and Obese Patients After Bariatric Surgery, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baylor University Medical Center, Farmer Branch, TX; 2Texas A&M School of Medicine, Sugar Land, TX; 3University of Texas, Arlington, TX; 4Baylor University Medical Center and Center for Esophageal Research, Baylor Scott & White Research Institute, Dallas, TX; 5Center for Esophageal Diseases, Baylor Scott & White Medical Center, Dallas, TX; 6Baylor Scott & White Center for Medical & Surgical Weight Loss Management, Dallas, TX; 7Baylor Scott & White Research Institute, Dallas, TX
Introduction: Several studies predating publication of Chicago Classification v4.0 (CCv4.0) found that high resolution manometry (HRM) often revealed motility disorders in obese patients who had bariatric surgery, but few data are available on HRM findings interpreted by CCv4.0 in obese patients. The primary aims of this study were to compare CCv4.0 motility diagnoses in obese patients undergoing evaluation for initial bariatric surgery with those who had undergone bariatric surgery, and to identify differences in CCv4.0 diagnoses among patients who had different types of bariatric surgery.
Methods: We analyzed our clinical database from April 2019 to March 2023 to identify obese patients who had HRM during evaluation for initial bariatric surgery (surgery-naïve group) or during evaluation after prior sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), or laparoscopic gastric band (LGB) surgery that resulted in insufficient weight loss (“postsurgical group”). Patients who had other foregut surgery besides SG, RYGB or LGB were excluded.
Results: We identified 48 surgery-naïve and 87 postsurgical patients (41 SG, 31 RYGB, 15 LGB). Presenting symptoms were: 58% dysphagia, 44% heartburn, 27% chest pain, 21% regurgitation, 7% other (abdominal pain, bloating, or nausea), 9% no symptoms. Compared to surgery-naïve patients, the median supine integrated relaxation pressure (IRP) was lower in SG (9.6 vs 13.6 mmHg, p=0.04) and RYGB patients (10.3 vs 13.6 mmHg, p=0.02), and higher in LGB patients (18.4 vs 13.6 mmHg, p=0.41) (Table 1). CCv4.0 manometric diagnoses were common across all four groups (Figure 1), particularly in LGB patients. Esophagogastric junction outflow obstruction (EGJOO) was the most frequent manometric diagnosis in surgery-naïve (27.1%), SG (17.1%), and LGB patients (60%), but was infrequent in RYGB patients (6.5%). Conversely, ineffective esophageal motility (IEM) was common in RYGB patients (19.4%) but rare in surgery-naïve (2.1%), SG (4.9%), and LGB (0%) patients. Compared to the surgery-naïve group, EGJOO was less frequent (p=0.02) and IEM was more frequent (p=0.01) in the RYGB patients.
Discussion: Esophageal motility disorders by CCv4.0 are common in obese patients, both before and after bariatric surgery. EGJOO is frequent in surgery-naïve, SG and LGB patients, but not in RYGB patients. Conversely, RYGB patients exhibit a higher frequency of IEM compared to the other groups. Further studies are needed to assess the clinical significance of these frequent manometric abnormalities.
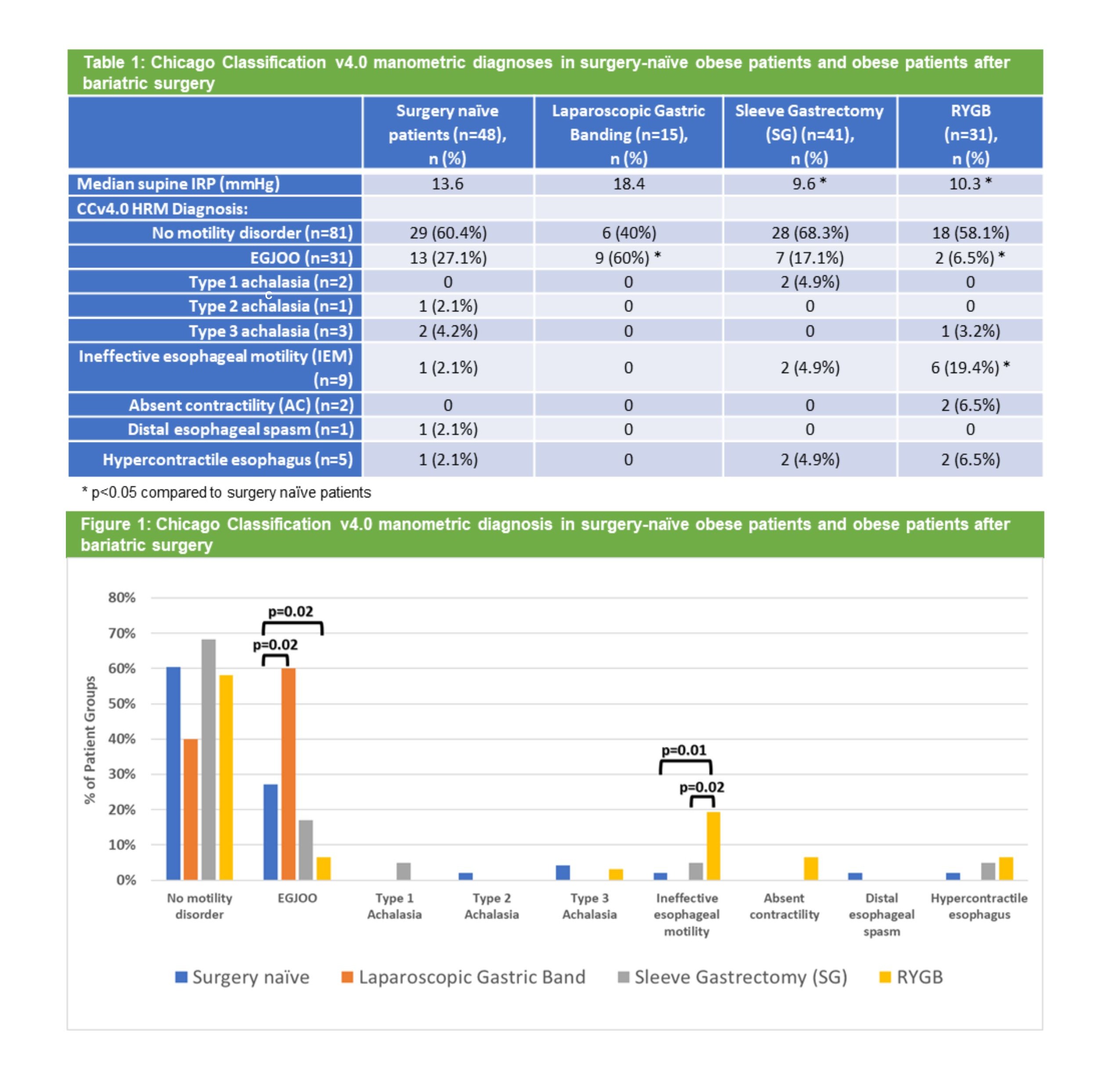
Figure: Table 1 and Figure 1: Chicago Classification v4.0 manometric diagnoses in surgery-naïve obese patients and obese patients after bariatric surgery
Disclosures:
Ambreen Anil Merchant indicated no relevant financial relationships.
Anjali Bhatt indicated no relevant financial relationships.
Daisha Cipher indicated no relevant financial relationships.
Ashton Ellison indicated no relevant financial relationships.
Chanakyaram Reddy indicated no relevant financial relationships.
Daniel Davis: Intuitive Surgical – Consultant.
Rhonda Souza: Capsulomics – Consultant. Castle Biosciences Inc – Consultant. Lucid Diagnostics – Consultant. Phathom Pharmaceuticals – Consultant. Sanofi – Grant/Research Support.
Vani Konda: Castle – Speakers Bureau. Exact – Advisory Committee/Board Member, Consultant. Medtronic – Advisory Committee/Board Member, Consultant. Pentax – Consultant. sebela – Advisor or Review Panel Member, Consultant.
Stuart Spechler: Castle Biosciences – Consultant. Lucid Diagnostics – Consultant. Phathom Pharmaceuticals – Consultant. Takeda Pharmaceuticals – Consultant.
Anh Nguyen indicated no relevant financial relationships.
Ambreen Anil Merchant, MD1, Anjali Bhatt, BS2, Daisha J.. Cipher, PhD3, Ashton Ellison, MBBCh4, Chanakyaram A.. Reddy, MD5, Daniel Davis, DO6, Rhonda F.. Souza, MD7, Vani J.A.. Konda, MD4, Stuart J.. Spechler, MD4, Anh D.. Nguyen, MD4. P0469 - Chicago Classification Version 4.0 Manometric Diagnoses in Surgery-Naïve Obese Patients and Obese Patients After Bariatric Surgery, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
