Sunday Poster Session
Category: Colon
P0387 - Tract on Fire: Lupus Enteritis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Christopher J. Costa, MD
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Christopher J. Costa, MD, Minh Thu T.. Nguyen, MD, Haleh Vaziri, MD
University of Connecticut Health Center, Farmington, CT
Introduction: Systemic lupus erythematosus (SLE) is an autoimmune condition that can affect multiple organ systems, including the GI tract. Diagnosing GI involvement is difficult due to nonspecific symptoms. An autopsy study found evidence of gastroenteritis in 70% of SLE patients, contrasting with clinical identification rates of only 10%.
Case Description/Methods: A 35-year-old female with long-standing SLE, including prior lupus nephritis, currently not on treatment, presented with acute nausea, vomiting, diarrhea, and abdominal pain. Her symptoms also included fever, chills, and malaise. She denied recent travel, antibiotic use, sick contacts, or substance use. Her vital signs included a temperature of 101°F, tachycardia to 155bpm, and normal blood pressure. On physical exam, she had decreased bowel sounds and diffuse tenderness with guarding. Her laboratory studies demonstrated: WBC 11.4*103/µL and unremarkable BMP and LFTs. She had low complement levels: C3 49mg/dL, C4 15mg/dL, and elevated serum inflammatory markers: ESR 23mm and CRP 97mg/L. Her anti-dsDNA test was moderately positive at 712IU/mL, a urine pregnancy test was negative.
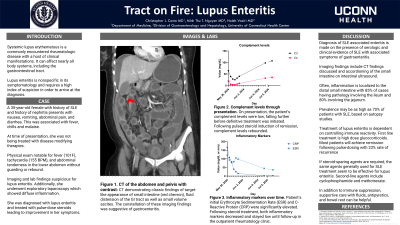
Abdominal CT imaging noted dilated bowel loops showing mucosal hyperenhancement and liquid stool and minor ascites suggestive of severe enterocolitis. She underwent explorative laparoscopy out of concern for a small bowel obstruction; only nonspecific enteritis was seen. Given her abnormal autoimmune labs and clinical presentation, lupus enterocolitis was diagnosed. She was treated with IV methylprednisolone 1g for three days, followed by 20mg every eight hours, resulting in rapid symptom improvement.
Discussion: Symptoms of lupus gastroenteritis include abdominal pain, nausea, vomiting, and diarrhea. The ileum and jejunum are involved in 85% and 80% of cases, respectively. Imaging findings include a “target-like” appearance of the small intestine on CT due to wall swelling, and an “accordion-like” appearance on intestinal ultrasound. When symptoms align with laboratory findings consistent with a lupus flare, diagnosis can be made clinically. The syndrome typically responds well to steroid treatment, with most patients achieving remission after pulse dose therapy. However, some cases may require adjunctive agents like cyclophosphamide or mycophenolate. This case illustrates a rare complication of a common autoimmune disorder, emphasizing the need for thorough clinical evaluation and accurate diagnosis. Once identified, prompt treatment yields favorable outcomes.

Disclosures:
Christopher J. Costa, MD, Minh Thu T.. Nguyen, MD, Haleh Vaziri, MD. P0387 - Tract on Fire: Lupus Enteritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Connecticut Health Center, Farmington, CT
Introduction: Systemic lupus erythematosus (SLE) is an autoimmune condition that can affect multiple organ systems, including the GI tract. Diagnosing GI involvement is difficult due to nonspecific symptoms. An autopsy study found evidence of gastroenteritis in 70% of SLE patients, contrasting with clinical identification rates of only 10%.
Case Description/Methods: A 35-year-old female with long-standing SLE, including prior lupus nephritis, currently not on treatment, presented with acute nausea, vomiting, diarrhea, and abdominal pain. Her symptoms also included fever, chills, and malaise. She denied recent travel, antibiotic use, sick contacts, or substance use. Her vital signs included a temperature of 101°F, tachycardia to 155bpm, and normal blood pressure. On physical exam, she had decreased bowel sounds and diffuse tenderness with guarding. Her laboratory studies demonstrated: WBC 11.4*103/µL and unremarkable BMP and LFTs. She had low complement levels: C3 49mg/dL, C4 15mg/dL, and elevated serum inflammatory markers: ESR 23mm and CRP 97mg/L. Her anti-dsDNA test was moderately positive at 712IU/mL, a urine pregnancy test was negative.
Abdominal CT imaging noted dilated bowel loops showing mucosal hyperenhancement and liquid stool and minor ascites suggestive of severe enterocolitis. She underwent explorative laparoscopy out of concern for a small bowel obstruction; only nonspecific enteritis was seen. Given her abnormal autoimmune labs and clinical presentation, lupus enterocolitis was diagnosed. She was treated with IV methylprednisolone 1g for three days, followed by 20mg every eight hours, resulting in rapid symptom improvement.
Discussion: Symptoms of lupus gastroenteritis include abdominal pain, nausea, vomiting, and diarrhea. The ileum and jejunum are involved in 85% and 80% of cases, respectively. Imaging findings include a “target-like” appearance of the small intestine on CT due to wall swelling, and an “accordion-like” appearance on intestinal ultrasound. When symptoms align with laboratory findings consistent with a lupus flare, diagnosis can be made clinically. The syndrome typically responds well to steroid treatment, with most patients achieving remission after pulse dose therapy. However, some cases may require adjunctive agents like cyclophosphamide or mycophenolate. This case illustrates a rare complication of a common autoimmune disorder, emphasizing the need for thorough clinical evaluation and accurate diagnosis. Once identified, prompt treatment yields favorable outcomes.

Figure: Abdominal CT with target-like appearance of small intestine as well as small volume ascites.
Disclosures:
Christopher Costa indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Haleh Vaziri indicated no relevant financial relationships.
Christopher J. Costa, MD, Minh Thu T.. Nguyen, MD, Haleh Vaziri, MD. P0387 - Tract on Fire: Lupus Enteritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
