Sunday Poster Session
Category: Colon
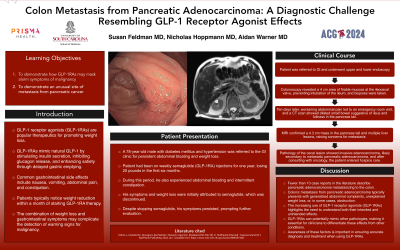
P0303 - Colon Metastasis From Pancreatic Adenocarcinoma: A Diagnostic Challenge Resembling GLP-1 Receptor Agonist Effects
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Susan Feldman, MD
Prisma Health, University of South Carolina School of Medicine
Columbia, SC
Presenting Author(s)
Susan Feldman, MD1, Aidan Warner, MD1, Nicholas Hoppmann, MD2
1Prisma Health, University of South Carolina School of Medicine, Columbia, SC; 2Columbia VA Health Care System, Columbia, SC
Introduction: GLP-1 receptor agonists (GLP-1RAs) have emerged as pivotal therapeutics for managing type 2 diabetes mellitus and facilitating weight loss. GLP-1RAs mimic endogenous GLP-1 by stimulating insulin secretion, inhibit glucagon release, and promote satiety via delayed gastric emptying. Despite its therapeutic efficacy, gastrointestinal adverse effects are common including nausea, vomiting, abdominal pain, constipation. Within a month of starting therapy, individuals notice the desired outcome of a reduction in weight. However, here lies a potential complication: the combination of weight loss and gastrointestinal symptoms may confound the onset alarm symptoms related to malignancy.
Case Description/Methods: Here we present a 78-year-old male with diabetes mellitus and hypertension referred to GI clinic due to persistent abdominal bloating and weight loss after stopping the GLP-1RA, semaglutide. One year prior, he began weekly semaglutide injections and noted a 20-pound weight loss during the first 6 months. He also experienced abdominal bloating and intermittent constipation. Initially symptoms and weight loss were attributed to semaglutide which was discontinued however his symptoms persisted. He was referred to GI and ultimately underwent upper and lower endoscopy. Colonoscopy revealed a 4 cm area of friable mucosa at the ileocecal valve preventing intubation of the ileum which was biopsied. Worsening of abdominal pain prompted an emergency room visit 10 days after colonoscopy. CT abdomen/pelvis showed dilated small bowel concerning for ileus as well as fullness in the tail of the pancreas. Subsequent MRI showed 4.3 cm mass in the tail of the pancreas with multiple liver lesion concerning for metastasis. Pathology from the cecal lesion demonstrated invasive adenocarcinoma in the colonic submucosa with focal colonization of the overlying colonic epithelium, likely secondary to metastatic pancreatic adenocarcinoma. After discussion with oncology, the patient and family went into hospice care.
Discussion: Though there are fewer than 10 case reports in the literature, pancreatic adenocarcinoma can metastasize to the colon. Typical presentation of colonic metastasis included generalized abdominal complaints, unexplained weight loss or in one case as obstruction. Given the increasing use of GLP-1RAs, it is important to understand the expected intended and unintended effects during its use as well at the potential to mimic other pathology.
Disclosures:
Susan Feldman, MD1, Aidan Warner, MD1, Nicholas Hoppmann, MD2. P0303 - Colon Metastasis From Pancreatic Adenocarcinoma: A Diagnostic Challenge Resembling GLP-1 Receptor Agonist Effects, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Prisma Health, University of South Carolina School of Medicine, Columbia, SC; 2Columbia VA Health Care System, Columbia, SC
Introduction: GLP-1 receptor agonists (GLP-1RAs) have emerged as pivotal therapeutics for managing type 2 diabetes mellitus and facilitating weight loss. GLP-1RAs mimic endogenous GLP-1 by stimulating insulin secretion, inhibit glucagon release, and promote satiety via delayed gastric emptying. Despite its therapeutic efficacy, gastrointestinal adverse effects are common including nausea, vomiting, abdominal pain, constipation. Within a month of starting therapy, individuals notice the desired outcome of a reduction in weight. However, here lies a potential complication: the combination of weight loss and gastrointestinal symptoms may confound the onset alarm symptoms related to malignancy.
Case Description/Methods: Here we present a 78-year-old male with diabetes mellitus and hypertension referred to GI clinic due to persistent abdominal bloating and weight loss after stopping the GLP-1RA, semaglutide. One year prior, he began weekly semaglutide injections and noted a 20-pound weight loss during the first 6 months. He also experienced abdominal bloating and intermittent constipation. Initially symptoms and weight loss were attributed to semaglutide which was discontinued however his symptoms persisted. He was referred to GI and ultimately underwent upper and lower endoscopy. Colonoscopy revealed a 4 cm area of friable mucosa at the ileocecal valve preventing intubation of the ileum which was biopsied. Worsening of abdominal pain prompted an emergency room visit 10 days after colonoscopy. CT abdomen/pelvis showed dilated small bowel concerning for ileus as well as fullness in the tail of the pancreas. Subsequent MRI showed 4.3 cm mass in the tail of the pancreas with multiple liver lesion concerning for metastasis. Pathology from the cecal lesion demonstrated invasive adenocarcinoma in the colonic submucosa with focal colonization of the overlying colonic epithelium, likely secondary to metastatic pancreatic adenocarcinoma. After discussion with oncology, the patient and family went into hospice care.
Discussion: Though there are fewer than 10 case reports in the literature, pancreatic adenocarcinoma can metastasize to the colon. Typical presentation of colonic metastasis included generalized abdominal complaints, unexplained weight loss or in one case as obstruction. Given the increasing use of GLP-1RAs, it is important to understand the expected intended and unintended effects during its use as well at the potential to mimic other pathology.
Disclosures:
Susan Feldman indicated no relevant financial relationships.
Aidan Warner indicated no relevant financial relationships.
Nicholas Hoppmann indicated no relevant financial relationships.
Susan Feldman, MD1, Aidan Warner, MD1, Nicholas Hoppmann, MD2. P0303 - Colon Metastasis From Pancreatic Adenocarcinoma: A Diagnostic Challenge Resembling GLP-1 Receptor Agonist Effects, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
