Sunday Poster Session
Category: Colon
P0314 - Simultaneous Clostridium Difficile Infection, Ulcerative Colitis and Colon Adenocarcinoma – Cause or Effect?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Samar Pal S. Sandhu, MBBS
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
Syed Mujtaba Baqir, MD1, Samar Pal S. Sandhu, MBBS1, Sarah Meribout, MD1, Neha Sharma, MBBS, MD1, Samantha S. Ehrlich, MD1, Tanuj Chokshi, DO2, Seth Lapin, DO1
1Maimonides Medical Center, Brooklyn, NY; 2Maimonides Medical Center, Clifton, NJ
Introduction: The burden of Clostridium difficile infection (CDI) is substantial not only in the general population but also in patients with inflammatory bowel disease (IBD). 76-79% IBD patients acquire CDI from the community. One study has shown clostridium difficile toxin B to promote colonic carcinogenesis. We present a case of a patient with recurrent CDI found to have undiagnosed IBD and colorectal cancer.
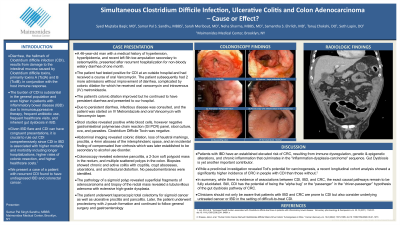
Case Description/Methods: A 46-year-old man with a past medical history of hypertension, hyperlipidemia, cirrhosis, recent left 5th toe osteomyelitis, presented after recurrent hospitalizations for watery, non-bloody diarrhea while on Levofloxacin. The patient had tested positive for CDI at an outside hospital and had received a course of oral Vancomycin. The patient subsequently had 2 more admissions without improvement of diarrhea, complicated by colonic dilation to 7.4 cm for which he received oral vancomycin and intravenous (IV) metronidazole. The patient’s colonic dilation improved. He then presented with persistent diarrhea. Stool studies revealed positive white blood cells, but negative gastrointestinal polymerase chain reaction panel, stool culture, ova and parasites. Clostridium Difficile Toxin was negative. Due to persistent diarrhea, patient was started on IV Metronidazole, Oral Vancomycin along with Vancomycin taper. Abdominal imaging with MRI revealed loss of haustral markings, proctitis and a 4mm abscess of the intersphincteric space. The colonoscopy revealed a large, soft polypoid mass in the rectum. Biopsies showed chronic and active colitis with cryptitis, crypt abscesses, and architectural distortion with rectal biopsy showing active colitis with ulcerations. No pseudomembranes identified. The pathology of the mass revealed a tubulovillous adenoma with extensive high-grade dysplasia. The patient underwent laparoscopic total abdominal colectomy and continued to follow general surgery and gastroenterology.
Discussion: Given IBD flare and CDI can have congruent presentations, it is crucial to rule out CDI comprehensively since there is a high risk of colectomy and increased mortality if immunosuppressive therapies are started without adequate antibiotic coverage for CDI. Our patient was young, not on any treatment for ulcerative colitis or any chemotherapy for cancer and had recurrent CDI. Clinicians should not only be aware that patients with both IBD and colorectal cancer are prone to CDI but also consider underlying untreated cancer or IBD in the setting of difficult to treat CDI.
Disclosures:
Syed Mujtaba Baqir, MD1, Samar Pal S. Sandhu, MBBS1, Sarah Meribout, MD1, Neha Sharma, MBBS, MD1, Samantha S. Ehrlich, MD1, Tanuj Chokshi, DO2, Seth Lapin, DO1. P0314 - Simultaneous Clostridium Difficile Infection, Ulcerative Colitis and Colon Adenocarcinoma – Cause or Effect?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Maimonides Medical Center, Brooklyn, NY; 2Maimonides Medical Center, Clifton, NJ
Introduction: The burden of Clostridium difficile infection (CDI) is substantial not only in the general population but also in patients with inflammatory bowel disease (IBD). 76-79% IBD patients acquire CDI from the community. One study has shown clostridium difficile toxin B to promote colonic carcinogenesis. We present a case of a patient with recurrent CDI found to have undiagnosed IBD and colorectal cancer.
Case Description/Methods: A 46-year-old man with a past medical history of hypertension, hyperlipidemia, cirrhosis, recent left 5th toe osteomyelitis, presented after recurrent hospitalizations for watery, non-bloody diarrhea while on Levofloxacin. The patient had tested positive for CDI at an outside hospital and had received a course of oral Vancomycin. The patient subsequently had 2 more admissions without improvement of diarrhea, complicated by colonic dilation to 7.4 cm for which he received oral vancomycin and intravenous (IV) metronidazole. The patient’s colonic dilation improved. He then presented with persistent diarrhea. Stool studies revealed positive white blood cells, but negative gastrointestinal polymerase chain reaction panel, stool culture, ova and parasites. Clostridium Difficile Toxin was negative. Due to persistent diarrhea, patient was started on IV Metronidazole, Oral Vancomycin along with Vancomycin taper. Abdominal imaging with MRI revealed loss of haustral markings, proctitis and a 4mm abscess of the intersphincteric space. The colonoscopy revealed a large, soft polypoid mass in the rectum. Biopsies showed chronic and active colitis with cryptitis, crypt abscesses, and architectural distortion with rectal biopsy showing active colitis with ulcerations. No pseudomembranes identified. The pathology of the mass revealed a tubulovillous adenoma with extensive high-grade dysplasia. The patient underwent laparoscopic total abdominal colectomy and continued to follow general surgery and gastroenterology.
Discussion: Given IBD flare and CDI can have congruent presentations, it is crucial to rule out CDI comprehensively since there is a high risk of colectomy and increased mortality if immunosuppressive therapies are started without adequate antibiotic coverage for CDI. Our patient was young, not on any treatment for ulcerative colitis or any chemotherapy for cancer and had recurrent CDI. Clinicians should not only be aware that patients with both IBD and colorectal cancer are prone to CDI but also consider underlying untreated cancer or IBD in the setting of difficult to treat CDI.
Disclosures:
Syed Mujtaba Baqir indicated no relevant financial relationships.
Samar Pal Sandhu indicated no relevant financial relationships.
Sarah Meribout indicated no relevant financial relationships.
Neha Sharma indicated no relevant financial relationships.
Samantha Ehrlich indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Seth Lapin indicated no relevant financial relationships.
Syed Mujtaba Baqir, MD1, Samar Pal S. Sandhu, MBBS1, Sarah Meribout, MD1, Neha Sharma, MBBS, MD1, Samantha S. Ehrlich, MD1, Tanuj Chokshi, DO2, Seth Lapin, DO1. P0314 - Simultaneous Clostridium Difficile Infection, Ulcerative Colitis and Colon Adenocarcinoma – Cause or Effect?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
