Sunday Poster Session
Category: Colon
P0315 - The Great Mimic: AL Amyloid in the Gastrointestinal Tract Impersonating Inflammatory Bowel Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KS
Katherine Shepherd, MD
West Virginia University
Morgantown, WV
Presenting Author(s)
Katherine Shepherd, MD1, Zach Kovach, MD1, Ethan M.. Cohen, MD1, Ayowumi Adekolu, MD1, Konstantinos Sdrimas, MD1, Kanwarpreet Tandon, MD2
1West Virginia University, Morgantown, WV; 2West Virginia University School of Medicine, Morgantown, WV
Introduction: AL amyloidosis is a plasma cell disorder with an uncontrolled production of immunoglobulin free light chains, and multiple myeloma (MM) is often the underlying disorder. Amyloid fibril deposition classically results in nephrotic syndrome and cardiomyopathy, and less commonly affects the gastrointestinal (GI) tract. AL amyloidosis of the GI tract presents with non-specific symptoms which may be misdiagnosed as a primary GI disorder.
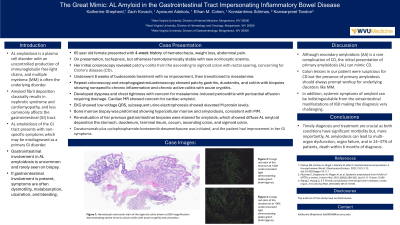
Case Description/Methods: A 65-year-old female presented with a 4-week history of hematochezia, weight loss, abdominal pain, and normocytic anemia. Her initial colonoscopy revealed patchy colitis from the ascending to sigmoid colon with rectal sparing, concerning for Crohn’s disease (CD). She showed minimal improvement after a trial of budesonide and was later transitioned to mesalamine while awaiting approval for biologic medication. However, she continued to have intermittent hematochezia and peripheral arthropathy. Upper endoscopy and repeat colonoscopy demonstrated patchy gastritis, duodenitis, and colitis with biopsies again showing nonspecific chronic inflammation and chronic active colitis with acute cryptitis. Shortly thereafter, she developed dyspnea and intermittent chest tightness concerning for mesalamine-induced pericarditis with pericardial effusion requiring drainage. Cardiac magnetic resolution imaging was suspicious for a new diagnosis of cardiac amyloid. Subsequent bone marrow biopsy showed M protein spike concerning for MM. A cardiac biopsy confirmed AL amyloidosis, and retrospective staining of previous GI biopsies revealed AL amyloidosis throughout the GI tract with low suspicion for CD per expert GI pathologist. Daratumumab plus cyclophosphamide-bortezomib-dexamethasone was initiated, and the patient had improvement in her GI symptoms.
Discussion: Although secondary amyloidosis (AA) is a rare complication of CD, the initial presentation of primary amyloidosis (AL) can mimic CD. Colon lesions in our patient were suspicious for CD but the presence of primary amyloidosis should always prompt workup for underlying disorders like MM. In addition, systemic symptoms of amyloid can be indistinguishable from the extraintestinal manifestations of IBD making the diagnosis very challenging. Timely diagnosis and treatment are crucial as both conditions have significant morbidity but, more importantly, AL amyloidosis can lead to multi-organ dysfunction, organ failure, and in 24–37% of patients, death within 6 months of diagnosis.
Disclosures:
Katherine Shepherd, MD1, Zach Kovach, MD1, Ethan M.. Cohen, MD1, Ayowumi Adekolu, MD1, Konstantinos Sdrimas, MD1, Kanwarpreet Tandon, MD2. P0315 - The Great Mimic: AL Amyloid in the Gastrointestinal Tract Impersonating Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1West Virginia University, Morgantown, WV; 2West Virginia University School of Medicine, Morgantown, WV
Introduction: AL amyloidosis is a plasma cell disorder with an uncontrolled production of immunoglobulin free light chains, and multiple myeloma (MM) is often the underlying disorder. Amyloid fibril deposition classically results in nephrotic syndrome and cardiomyopathy, and less commonly affects the gastrointestinal (GI) tract. AL amyloidosis of the GI tract presents with non-specific symptoms which may be misdiagnosed as a primary GI disorder.
Case Description/Methods: A 65-year-old female presented with a 4-week history of hematochezia, weight loss, abdominal pain, and normocytic anemia. Her initial colonoscopy revealed patchy colitis from the ascending to sigmoid colon with rectal sparing, concerning for Crohn’s disease (CD). She showed minimal improvement after a trial of budesonide and was later transitioned to mesalamine while awaiting approval for biologic medication. However, she continued to have intermittent hematochezia and peripheral arthropathy. Upper endoscopy and repeat colonoscopy demonstrated patchy gastritis, duodenitis, and colitis with biopsies again showing nonspecific chronic inflammation and chronic active colitis with acute cryptitis. Shortly thereafter, she developed dyspnea and intermittent chest tightness concerning for mesalamine-induced pericarditis with pericardial effusion requiring drainage. Cardiac magnetic resolution imaging was suspicious for a new diagnosis of cardiac amyloid. Subsequent bone marrow biopsy showed M protein spike concerning for MM. A cardiac biopsy confirmed AL amyloidosis, and retrospective staining of previous GI biopsies revealed AL amyloidosis throughout the GI tract with low suspicion for CD per expert GI pathologist. Daratumumab plus cyclophosphamide-bortezomib-dexamethasone was initiated, and the patient had improvement in her GI symptoms.
Discussion: Although secondary amyloidosis (AA) is a rare complication of CD, the initial presentation of primary amyloidosis (AL) can mimic CD. Colon lesions in our patient were suspicious for CD but the presence of primary amyloidosis should always prompt workup for underlying disorders like MM. In addition, systemic symptoms of amyloid can be indistinguishable from the extraintestinal manifestations of IBD making the diagnosis very challenging. Timely diagnosis and treatment are crucial as both conditions have significant morbidity but, more importantly, AL amyloidosis can lead to multi-organ dysfunction, organ failure, and in 24–37% of patients, death within 6 months of diagnosis.
Disclosures:
Katherine Shepherd indicated no relevant financial relationships.
Zach Kovach indicated no relevant financial relationships.
Ethan Cohen indicated no relevant financial relationships.
Ayowumi Adekolu indicated no relevant financial relationships.
Konstantinos Sdrimas indicated no relevant financial relationships.
Kanwarpreet Tandon indicated no relevant financial relationships.
Katherine Shepherd, MD1, Zach Kovach, MD1, Ethan M.. Cohen, MD1, Ayowumi Adekolu, MD1, Konstantinos Sdrimas, MD1, Kanwarpreet Tandon, MD2. P0315 - The Great Mimic: AL Amyloid in the Gastrointestinal Tract Impersonating Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

