Sunday Poster Session
Category: Colon
P0220 - In-Patient Analysis of Colonic Mesenteric Ischemia Among COVID-19 Hospitalizations: A Population-Based Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Anwar Uddin, MD
SUNY Downstate Medical Center
Brooklyn, NY
Presenting Author(s)
Anwar Uddin, MD1, Prashil Dave, MD2, Peter Lymberopoulos, MD1, Justin Chung, MD3, Madia Ahad, MD1, Rafat Uddin, BA1, Rahat Uddin, MS1, Afgal Ahad, MD1, Syeda M. Ali, MD1
1SUNY Downstate Medical Center, Brooklyn, NY; 2State University of New York Downstate, Brooklyn, NY; 3SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Covid-19 infection predispose to increase risk of thrombosis and ischemia and can potentially lead to intestinal ischemia with worst outcomes. We conducted a nationwide study to examine the prevalence and inpatient outcomes of colonic mesenteric ischemia (CMI) in covid-19 patients using the nationwide database.
Methods: We used the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS) to identify adult patients admitted with covid-19 infection in 2020 using ICD-10-CM codes (U.071, U.00, U.49, U.50, U.85, J.1282, and B.342). We used ICD-10-CM codes to identify patients with CMI (K55.0x). Main outcomes were in-hospital mortality, length of stay (LOS), and hospital costs. We evaluate the association between acute diverticulitis and outcomes using survey based multivariate logistic regression models for in-hospital mortality, Poisson regression for LOS, and generalized linear model with gamma distribution and log link for hospitalization cost. Models were adjusted for age, sex, race and ethnicity, primary payer, Charlson comorbidity index, hospital bed size, hospital region and hospital teaching status.
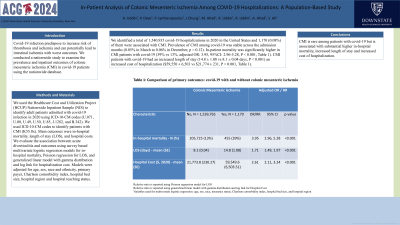
Results: We identified a total of 1,540,935 covid-19 hospitalizations in 2020 in the United States and 1,170 (0.08%) of them were associated with CMI. Prevalence of CMI among covid-19 was stable across the admission months (0.05% in March to 0.06% in December, p = 0.12). In‐patient mortality was significantly higher in CMI patients with covid-19 (39% vs 13%, adjusted OR: 3.95, 95%CI: 2.96-5.28, P < 0.001, Table 1). CMI patients with covid-19 had an increased length of stay (14.8 ± 1.08 vs 8.1 ± 0.04 days, P < 0.001) an increased cost of hospitalization ($59,550 ± 6,503 vs $21,774 ± 231, P < 0.001, Table 1).
Discussion: CMI is rare among patients with covid-19 but is associated with substantial higher in‐hospital mortality, increased length of stay and increased cost of hospitalization.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anwar Uddin, MD1, Prashil Dave, MD2, Peter Lymberopoulos, MD1, Justin Chung, MD3, Madia Ahad, MD1, Rafat Uddin, BA1, Rahat Uddin, MS1, Afgal Ahad, MD1, Syeda M. Ali, MD1. P0220 - In-Patient Analysis of Colonic Mesenteric Ischemia Among COVID-19 Hospitalizations: A Population-Based Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SUNY Downstate Medical Center, Brooklyn, NY; 2State University of New York Downstate, Brooklyn, NY; 3SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Covid-19 infection predispose to increase risk of thrombosis and ischemia and can potentially lead to intestinal ischemia with worst outcomes. We conducted a nationwide study to examine the prevalence and inpatient outcomes of colonic mesenteric ischemia (CMI) in covid-19 patients using the nationwide database.
Methods: We used the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS) to identify adult patients admitted with covid-19 infection in 2020 using ICD-10-CM codes (U.071, U.00, U.49, U.50, U.85, J.1282, and B.342). We used ICD-10-CM codes to identify patients with CMI (K55.0x). Main outcomes were in-hospital mortality, length of stay (LOS), and hospital costs. We evaluate the association between acute diverticulitis and outcomes using survey based multivariate logistic regression models for in-hospital mortality, Poisson regression for LOS, and generalized linear model with gamma distribution and log link for hospitalization cost. Models were adjusted for age, sex, race and ethnicity, primary payer, Charlson comorbidity index, hospital bed size, hospital region and hospital teaching status.
Results: We identified a total of 1,540,935 covid-19 hospitalizations in 2020 in the United States and 1,170 (0.08%) of them were associated with CMI. Prevalence of CMI among covid-19 was stable across the admission months (0.05% in March to 0.06% in December, p = 0.12). In‐patient mortality was significantly higher in CMI patients with covid-19 (39% vs 13%, adjusted OR: 3.95, 95%CI: 2.96-5.28, P < 0.001, Table 1). CMI patients with covid-19 had an increased length of stay (14.8 ± 1.08 vs 8.1 ± 0.04 days, P < 0.001) an increased cost of hospitalization ($59,550 ± 6,503 vs $21,774 ± 231, P < 0.001, Table 1).
Discussion: CMI is rare among patients with covid-19 but is associated with substantial higher in‐hospital mortality, increased length of stay and increased cost of hospitalization.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anwar Uddin indicated no relevant financial relationships.
Prashil Dave indicated no relevant financial relationships.
Peter Lymberopoulos indicated no relevant financial relationships.
Justin Chung indicated no relevant financial relationships.
Madia Ahad indicated no relevant financial relationships.
Rafat Uddin indicated no relevant financial relationships.
Rahat Uddin indicated no relevant financial relationships.
Afgal Ahad indicated no relevant financial relationships.
Syeda Ali indicated no relevant financial relationships.
Anwar Uddin, MD1, Prashil Dave, MD2, Peter Lymberopoulos, MD1, Justin Chung, MD3, Madia Ahad, MD1, Rafat Uddin, BA1, Rahat Uddin, MS1, Afgal Ahad, MD1, Syeda M. Ali, MD1. P0220 - In-Patient Analysis of Colonic Mesenteric Ischemia Among COVID-19 Hospitalizations: A Population-Based Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
