Sunday Poster Session
Category: Colon
P0222 - Investigating Fecal Calprotectin: Unmasking the Sneaky Subtypes of Non-IBD Colitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Abdulmalik Saleem, MD
Henry Ford Health
Flushing, MI
Presenting Author(s)
Award: Presidential Poster Award
Abdulmalik Saleem, MD1, Allison N. Malick, MD1, Ahmad Alomari, MD2, Muhammad Saad Faisal, MD1, Mohammed Abusuliman, MD1, Sheema Rehman, DO2, Ammad Javaid. Chaudhary, MD1, Ahmed M. Ibrahim, MD3, Taher Jamali, MD2, Suraj Suresh, MD1
1Henry Ford Health, Detroit, MI; 2Henry Ford Hospital, Detroit, MI; 3Trinity Health Ann Arbor Hospital, Ypsilanti, MI
Introduction: The current gold standard for diagnosing non-IBD colitis is colonoscopy with biopsy. Imaging and stool-based tests are also often utilized during initial evaluation to screen for intestinal inflammation. Fecal calprotectin (FC) is a sensitive marker in assessing IBD disease activity, but its utility in non-IBD colitis has not been extensively evaluated. In this study, we aim to assess the utility of fecal calprotectin as a screening test for various subtypes of non-IBD colitis.
Methods: This was a retrospective study of clinic patients at a tertiary care medical system who presented with subacute or chronic diarrhea between 2013-2023. Patients who had an abnormal FC during their clinic visit and underwent a colonoscopy within 3 months of this test result were included. Patients with a new or prior diagnosis of IBD or infectious colitis were excluded. Baseline patient characteristics, FC levels, histologic, and endoscopic findings on colonoscopy were collected from medical records. FC levels in patients with non-IBD colitis were compared to those without colitis.
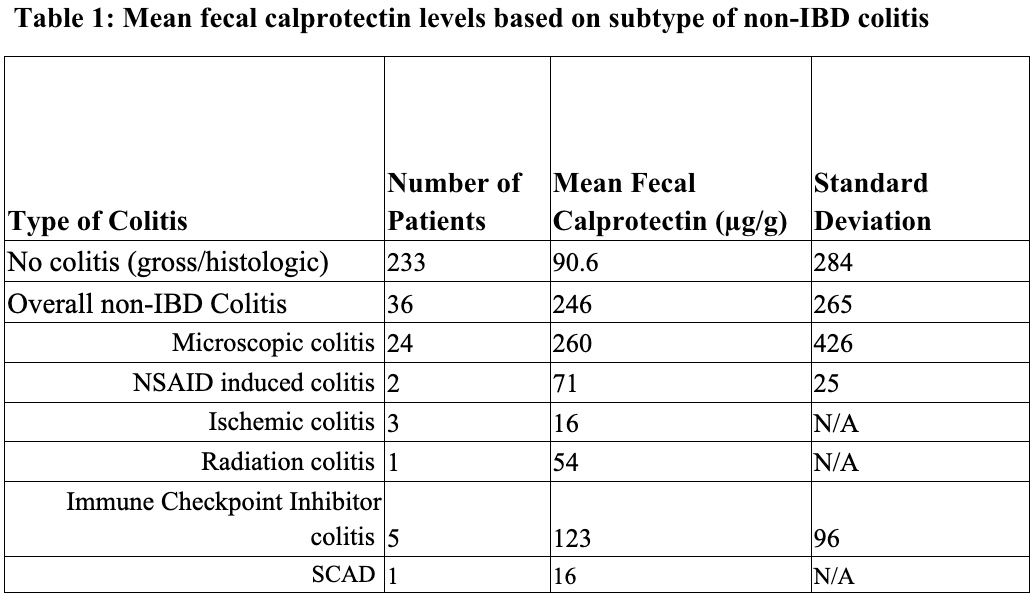
Results: 282 patients met our inclusion criteria, of which 36 had specific types of non-IBD colitis diagnosed based on histology. These clinical subtypes included microscopic colitis (66%), immune checkpoint inhibitor (ICI) colitis (14%), NSAID induced colitis (6%), ischemic colitis (8%), radiation colitis (3%), and segmental colitis associated with diverticulosis (SCAD) (3%) (Table 1). 233 patients had no gross or histologic features of colitis. The mean FC level of patients with a specific clinical subtype of non-IBD colitis was 246 (SD 265) compared to 90 (SD 284) in patients without colitis. Table 1 shows the mean FC levels of patients diagnosed with each clinical sub-type of non-IBD colitis. A Mann-Whitney test was performed demonstrating a significant difference in these two groups (p < 0.001).
Discussion: Our study demonstrates a significant quantitative difference in FC level between patients with non-IBD colitis and those without colitis. However, this difference was primarily seen in patients with microscopic colitis and ICI colitis whereas patients with NSAID induced, ischemic, radiation colitis, and SCAD had FC levels similar to patients without colitis. These preliminary findings suggest that although FC shows promise as a screening marker for non-IBD colitis, clinicians should not rely too heavily on this test, especially when a patient has risk factors for a specific type of colitis.
Disclosures:
Abdulmalik Saleem, MD1, Allison N. Malick, MD1, Ahmad Alomari, MD2, Muhammad Saad Faisal, MD1, Mohammed Abusuliman, MD1, Sheema Rehman, DO2, Ammad Javaid. Chaudhary, MD1, Ahmed M. Ibrahim, MD3, Taher Jamali, MD2, Suraj Suresh, MD1. P0222 - Investigating Fecal Calprotectin: Unmasking the Sneaky Subtypes of Non-IBD Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Abdulmalik Saleem, MD1, Allison N. Malick, MD1, Ahmad Alomari, MD2, Muhammad Saad Faisal, MD1, Mohammed Abusuliman, MD1, Sheema Rehman, DO2, Ammad Javaid. Chaudhary, MD1, Ahmed M. Ibrahim, MD3, Taher Jamali, MD2, Suraj Suresh, MD1
1Henry Ford Health, Detroit, MI; 2Henry Ford Hospital, Detroit, MI; 3Trinity Health Ann Arbor Hospital, Ypsilanti, MI
Introduction: The current gold standard for diagnosing non-IBD colitis is colonoscopy with biopsy. Imaging and stool-based tests are also often utilized during initial evaluation to screen for intestinal inflammation. Fecal calprotectin (FC) is a sensitive marker in assessing IBD disease activity, but its utility in non-IBD colitis has not been extensively evaluated. In this study, we aim to assess the utility of fecal calprotectin as a screening test for various subtypes of non-IBD colitis.
Methods: This was a retrospective study of clinic patients at a tertiary care medical system who presented with subacute or chronic diarrhea between 2013-2023. Patients who had an abnormal FC during their clinic visit and underwent a colonoscopy within 3 months of this test result were included. Patients with a new or prior diagnosis of IBD or infectious colitis were excluded. Baseline patient characteristics, FC levels, histologic, and endoscopic findings on colonoscopy were collected from medical records. FC levels in patients with non-IBD colitis were compared to those without colitis.
Results: 282 patients met our inclusion criteria, of which 36 had specific types of non-IBD colitis diagnosed based on histology. These clinical subtypes included microscopic colitis (66%), immune checkpoint inhibitor (ICI) colitis (14%), NSAID induced colitis (6%), ischemic colitis (8%), radiation colitis (3%), and segmental colitis associated with diverticulosis (SCAD) (3%) (Table 1). 233 patients had no gross or histologic features of colitis. The mean FC level of patients with a specific clinical subtype of non-IBD colitis was 246 (SD 265) compared to 90 (SD 284) in patients without colitis. Table 1 shows the mean FC levels of patients diagnosed with each clinical sub-type of non-IBD colitis. A Mann-Whitney test was performed demonstrating a significant difference in these two groups (p < 0.001).
Discussion: Our study demonstrates a significant quantitative difference in FC level between patients with non-IBD colitis and those without colitis. However, this difference was primarily seen in patients with microscopic colitis and ICI colitis whereas patients with NSAID induced, ischemic, radiation colitis, and SCAD had FC levels similar to patients without colitis. These preliminary findings suggest that although FC shows promise as a screening marker for non-IBD colitis, clinicians should not rely too heavily on this test, especially when a patient has risk factors for a specific type of colitis.
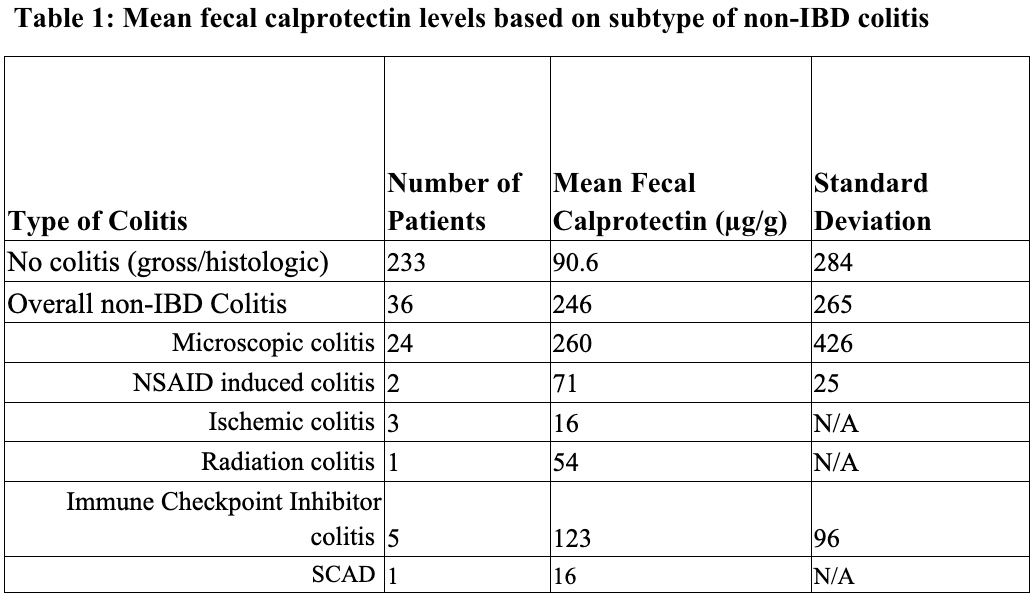
Figure: Table 1: Mean fecal calprotectin levels based on subtype of non-IBD colitis
Disclosures:
Abdulmalik Saleem indicated no relevant financial relationships.
Allison Malick indicated no relevant financial relationships.
Ahmad Alomari indicated no relevant financial relationships.
Muhammad Saad Faisal indicated no relevant financial relationships.
Mohammed Abusuliman indicated no relevant financial relationships.
Sheema Rehman indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Ahmed Ibrahim indicated no relevant financial relationships.
Taher Jamali indicated no relevant financial relationships.
Suraj Suresh indicated no relevant financial relationships.
Abdulmalik Saleem, MD1, Allison N. Malick, MD1, Ahmad Alomari, MD2, Muhammad Saad Faisal, MD1, Mohammed Abusuliman, MD1, Sheema Rehman, DO2, Ammad Javaid. Chaudhary, MD1, Ahmed M. Ibrahim, MD3, Taher Jamali, MD2, Suraj Suresh, MD1. P0222 - Investigating Fecal Calprotectin: Unmasking the Sneaky Subtypes of Non-IBD Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

