Sunday Poster Session
Category: Biliary/Pancreas
P0163 - A Case of Abdominal Wall Pain Misdiagnosed as Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- TL
Tayna Latortue, MD
University of Florida
Gainesville, FL
Presenting Author(s)
Tayna Latortue, MD1, Andrew Kleehammer, DO2, Bashar Qumseya, MD, MPH2
1University of Florida, Gainesville, FL; 2University of Florida College of Medicine, Gainesville, FL
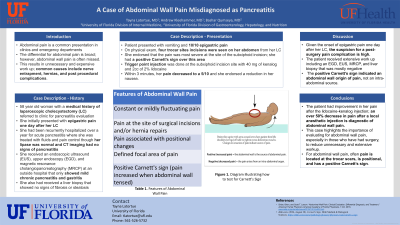
Introduction: Abdominal pain is a common presentation in clinics and emergency departments (ED). The differential for abdominal pain is broad; however, abdominal wall pain is often missed. This results in unnecessary and expensive work up; common causes include nerve entrapment, hernias, and post procedural complications.
Case Description/Methods: A 58-year-old woman with a history of a laparoscopic cholecystectomy (LC) a year ago was referred to clinic for pancreatitis. She initially had epigastric pain one day after her LC. She had an upper endoscopy (EGD) that showed gastritis. Due to concern for pancreatitis and unexplained pain, she had an endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP) that showed only mild chronic pancreatitis. She was hospitalized for the same pain 6 months later for pancreatitis. She was evaluated for hepatitis during the admission and received a liver biopsy; no fibrosis and steatosis was seen. She went to the ED 5 times over the past few months for her pain and was repeatedly diagnosed with acute pancreatitis, though her lipase was normal, and CT showed no signs of pancreatitis. She was given fluids, pain control and sent home. In clinic, she was vomiting and endorsing 10/10 epigastric pain. On physical exam, four trocar site incisions were seen from her LC. She endorsed that her pain was most severe at the site of her subxiphoid incision. She had a positive Carnett’s sign over this area Trigger point injection of the site was done with 40mg of kenelog and 2cc of 2% lidocaine. Within 3 minutes, her pain decreased to a 5/10. She was referred to a pain specialist for trigger point injections as needed.
Discussion: Given the onset of epigastric pain one day after her LC, the suspicion for a post-surgery pain complication is high. The patient received extensive work up including an EGD, EUS, MRCP, and liver biopsy. She had persistent pain that was only temporarily relieved during her ED visits when she was given fluids and pain control. The positive Carnett’s sign indicated an abdominal wall origin of pain, not an intra-abdominal source. The patient had improvement in her pain after the lidocaine-kenolog injection; an over 50% decrease in pain after a local anesthetic injection is diagnostic of abdominal wall pain. This case highlights the importance of evaluating for abdominal wall pain, especially in those who have had surgery. For abdominal wall pain, often pain is located at the trocar scars, is positional, and has a positive Carnett’s sign.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tayna Latortue, MD1, Andrew Kleehammer, DO2, Bashar Qumseya, MD, MPH2. P0163 - A Case of Abdominal Wall Pain Misdiagnosed as Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Florida, Gainesville, FL; 2University of Florida College of Medicine, Gainesville, FL
Introduction: Abdominal pain is a common presentation in clinics and emergency departments (ED). The differential for abdominal pain is broad; however, abdominal wall pain is often missed. This results in unnecessary and expensive work up; common causes include nerve entrapment, hernias, and post procedural complications.
Case Description/Methods: A 58-year-old woman with a history of a laparoscopic cholecystectomy (LC) a year ago was referred to clinic for pancreatitis. She initially had epigastric pain one day after her LC. She had an upper endoscopy (EGD) that showed gastritis. Due to concern for pancreatitis and unexplained pain, she had an endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP) that showed only mild chronic pancreatitis. She was hospitalized for the same pain 6 months later for pancreatitis. She was evaluated for hepatitis during the admission and received a liver biopsy; no fibrosis and steatosis was seen. She went to the ED 5 times over the past few months for her pain and was repeatedly diagnosed with acute pancreatitis, though her lipase was normal, and CT showed no signs of pancreatitis. She was given fluids, pain control and sent home. In clinic, she was vomiting and endorsing 10/10 epigastric pain. On physical exam, four trocar site incisions were seen from her LC. She endorsed that her pain was most severe at the site of her subxiphoid incision. She had a positive Carnett’s sign over this area Trigger point injection of the site was done with 40mg of kenelog and 2cc of 2% lidocaine. Within 3 minutes, her pain decreased to a 5/10. She was referred to a pain specialist for trigger point injections as needed.
Discussion: Given the onset of epigastric pain one day after her LC, the suspicion for a post-surgery pain complication is high. The patient received extensive work up including an EGD, EUS, MRCP, and liver biopsy. She had persistent pain that was only temporarily relieved during her ED visits when she was given fluids and pain control. The positive Carnett’s sign indicated an abdominal wall origin of pain, not an intra-abdominal source. The patient had improvement in her pain after the lidocaine-kenolog injection; an over 50% decrease in pain after a local anesthetic injection is diagnostic of abdominal wall pain. This case highlights the importance of evaluating for abdominal wall pain, especially in those who have had surgery. For abdominal wall pain, often pain is located at the trocar scars, is positional, and has a positive Carnett’s sign.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tayna Latortue indicated no relevant financial relationships.
Andrew Kleehammer indicated no relevant financial relationships.
Bashar Qumseya indicated no relevant financial relationships.
Tayna Latortue, MD1, Andrew Kleehammer, DO2, Bashar Qumseya, MD, MPH2. P0163 - A Case of Abdominal Wall Pain Misdiagnosed as Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
