Sunday Poster Session
Category: Biliary/Pancreas
P0164 - Sump Syndrome - Diagnosis Dilemmas and Therapeutic Approaches: A Case Series
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Shahem Abbarah, MD
MedStar Health
Baltimore, MD
Presenting Author(s)
Award: Presidential Poster Award
Shahem Abbarah, MD1, Mhd Kutaiba Albuni, MD2, Bisher Sawaf, MD3, Bana Sabbagh, MD4, Abdellatif Ismail, MD5, Hussam Almasri, MD6
1MedStar Health, Baltimore, MD; 2TriHealth, Doha, Ad Dawhah, Qatar; 3University of Toledo, Toledo, OH; 4TriHealth, Cincinnati, OH; 5University of Maryland Medical Center, Baltimore, MD
Introduction: Sump syndrome is a rare and often long-term complication of choledochoduodenostomy (CDD). The presentation and severity are variable, and management should be tailored to each patient based on several factors. Herein, we report three cases of Sump syndrome, each demonstrating unique diagnostic dilemmas and therapeutic modalities.
Case Description/Methods: Case I. A 35-year-old woman presented to the emergency department with right upper quadrant abdominal pain, nausea, vomiting, and yellowish skin discoloration. She had a history of open cholecystectomy two years prior. Examination revealed febrile, tachycardic, and hypotensive vitals, as well as diffuse abdominal tenderness. Blood tests showed high inflammatory markers, and liver function tests showed a cholestatic picture. Imaging revealed features of acute ascending cholangitis, and a decision was made for percutaneous transhepatic cholangiography. Endoscopy showed a common bile duct stone in the duodenum, which was removed. The patient recovered after treatment and a 30-day hospital stay.
Case II. The second case is a 52-year-old woman with a history of hypertension and open cholecystectomy at the age of 30. She presented to the ED with epigastric pain, vomiting, and unstable vital signs. Labs showed high inflammatory markers and liver enzyme levels, and imaging revealed gallstones and a choledocho-duodenal fistula. She developed chest pain and was diagnosed with type II myocardial infarction. Following biliary decompression and treatment, the patient improved and was discharged home.
Case III. A 65-year-old Pakistani man with a history of diabetes mellitus, hypertension, coronary artery disease, and cholecystectomy had recurrent visits to the ED due to upper abdominal pain and nausea. His CT was unremarkable, but US showed intrahepatic pneumobilia. Endoscopy revealed anatomical evidence of CDD, and he was diagnosed with sump syndrome. He was planned for ERCP as an outpatient but did not attend the appointment.
Discussion: Sump syndrome is an uncommon late complication of CDD. It is important to consider the diagnosis in patients with a history of open cholecystectomy, particularly in those who migrate from developing countries. The presentation may range from acute severe, mimicking acute ascending cholangitis, to chronic recurrent abdominal pain without evidence of inflammation. Management is a case-by-case decision, with principal management aims to decompress the biliary tract and address any underlying sepsis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shahem Abbarah, MD1, Mhd Kutaiba Albuni, MD2, Bisher Sawaf, MD3, Bana Sabbagh, MD4, Abdellatif Ismail, MD5. P0164 - Sump Syndrome - Diagnosis Dilemmas and Therapeutic Approaches: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Shahem Abbarah, MD1, Mhd Kutaiba Albuni, MD2, Bisher Sawaf, MD3, Bana Sabbagh, MD4, Abdellatif Ismail, MD5, Hussam Almasri, MD6
1MedStar Health, Baltimore, MD; 2TriHealth, Doha, Ad Dawhah, Qatar; 3University of Toledo, Toledo, OH; 4TriHealth, Cincinnati, OH; 5University of Maryland Medical Center, Baltimore, MD
Introduction: Sump syndrome is a rare and often long-term complication of choledochoduodenostomy (CDD). The presentation and severity are variable, and management should be tailored to each patient based on several factors. Herein, we report three cases of Sump syndrome, each demonstrating unique diagnostic dilemmas and therapeutic modalities.
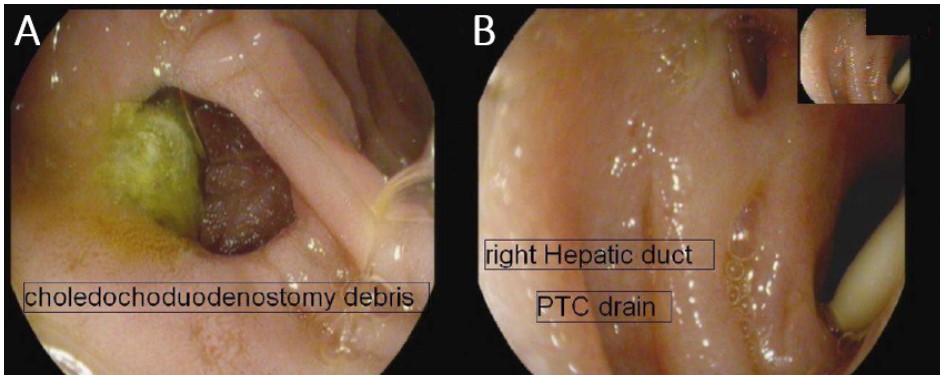
Case Description/Methods: Case I. A 35-year-old woman presented to the emergency department with right upper quadrant abdominal pain, nausea, vomiting, and yellowish skin discoloration. She had a history of open cholecystectomy two years prior. Examination revealed febrile, tachycardic, and hypotensive vitals, as well as diffuse abdominal tenderness. Blood tests showed high inflammatory markers, and liver function tests showed a cholestatic picture. Imaging revealed features of acute ascending cholangitis, and a decision was made for percutaneous transhepatic cholangiography. Endoscopy showed a common bile duct stone in the duodenum, which was removed. The patient recovered after treatment and a 30-day hospital stay.
Case II. The second case is a 52-year-old woman with a history of hypertension and open cholecystectomy at the age of 30. She presented to the ED with epigastric pain, vomiting, and unstable vital signs. Labs showed high inflammatory markers and liver enzyme levels, and imaging revealed gallstones and a choledocho-duodenal fistula. She developed chest pain and was diagnosed with type II myocardial infarction. Following biliary decompression and treatment, the patient improved and was discharged home.
Case III. A 65-year-old Pakistani man with a history of diabetes mellitus, hypertension, coronary artery disease, and cholecystectomy had recurrent visits to the ED due to upper abdominal pain and nausea. His CT was unremarkable, but US showed intrahepatic pneumobilia. Endoscopy revealed anatomical evidence of CDD, and he was diagnosed with sump syndrome. He was planned for ERCP as an outpatient but did not attend the appointment.
Discussion: Sump syndrome is an uncommon late complication of CDD. It is important to consider the diagnosis in patients with a history of open cholecystectomy, particularly in those who migrate from developing countries. The presentation may range from acute severe, mimicking acute ascending cholangitis, to chronic recurrent abdominal pain without evidence of inflammation. Management is a case-by-case decision, with principal management aims to decompress the biliary tract and address any underlying sepsis.
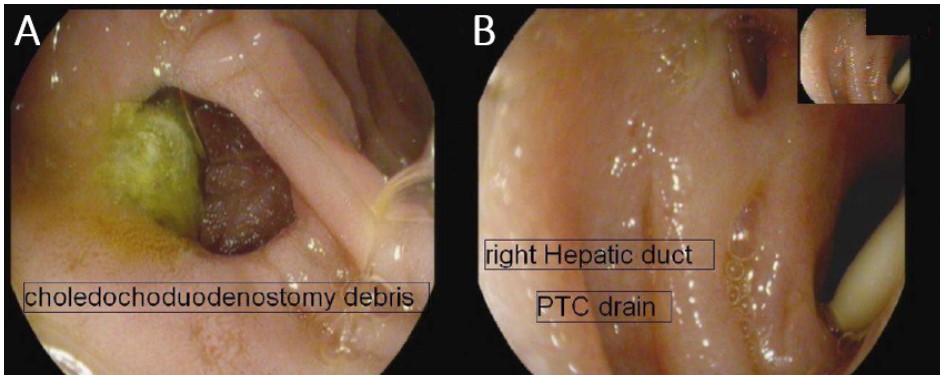
Figure: Forword endoscopic view of the first patient demonstrating: A. choledochoduodenostomy (CDD) with debris visualized. B. Right hepatic duct with percutaneous transhepatic cholangiography (PTC) drain in place.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shahem Abbarah indicated no relevant financial relationships.
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Bana Sabbagh indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Shahem Abbarah, MD1, Mhd Kutaiba Albuni, MD2, Bisher Sawaf, MD3, Bana Sabbagh, MD4, Abdellatif Ismail, MD5. P0164 - Sump Syndrome - Diagnosis Dilemmas and Therapeutic Approaches: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

