Sunday Poster Session
Category: Biliary/Pancreas
P0074 - Chronic Hepatobiliary Brucellosis With the Novel Development of Focal Invasive Ampullary Adenocarcinoma: A Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Zachary C. Vinton, DO
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Zachary C. Vinton, DO1, Kevin Wolfe, DO2, Matthew Stotts, MD, MPH3, Mark Rosenblatt, MD4, Clark Kulig, MD3, Kathy Sotelo, MD3, Thomas Heffron, MD3, Vimal Jhaveri, MD3
1University of Nebraska Medical Center, Omaha, NE; 2Hennepin Healthcare, Minneapolis, MN; 3Presbyterian/St. Luke's Medical Center, Denver, CO; 4UCHealth Longmont, Longmont, CO
Introduction: Brucellosis is a zoonotic bacterial infection with a long and recurrent course of disease. While biliary complications can occur, there are no reported cases of biliary dysplasia or gastrointestinal malignancy associated with brucellosis.
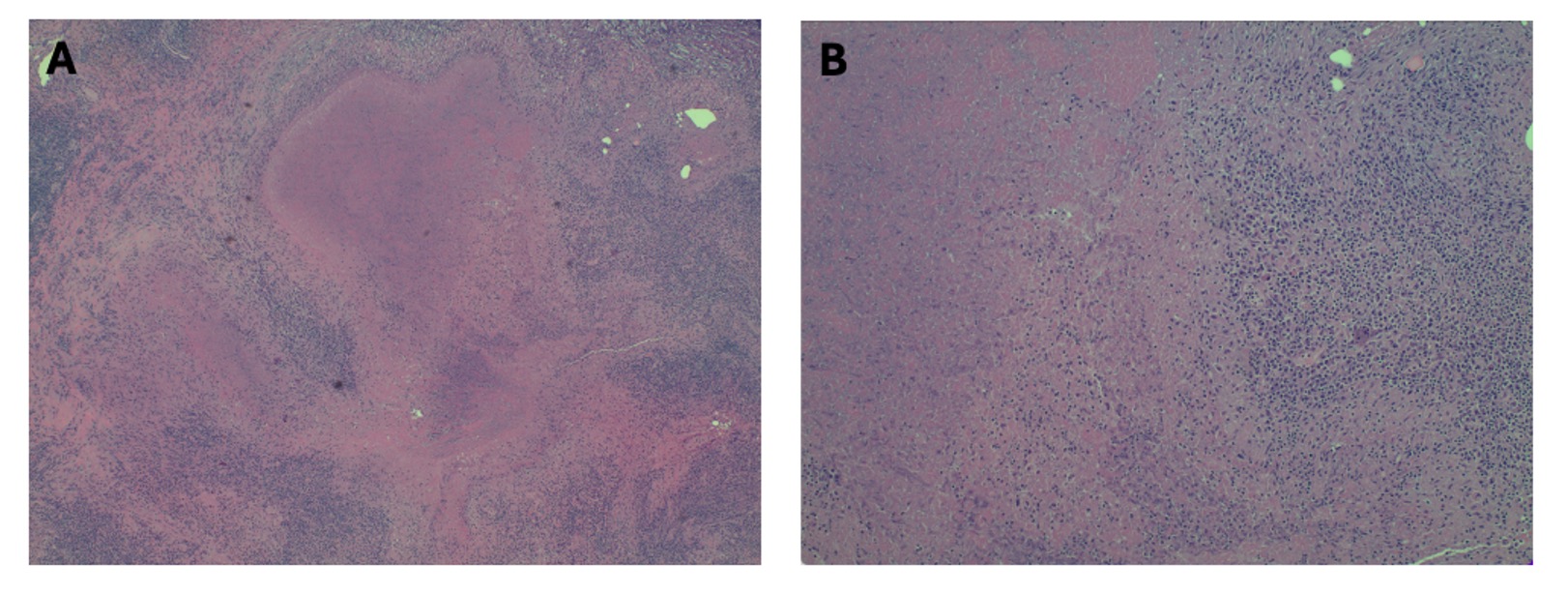
Case Description/Methods: A 68-year-old male with a history of cholecystitis requiring cholecystectomy presented with 18 months of night sweats, headaches, intermittent fevers, muscle wasting, and weight loss. Multiple ERCPs were performed revealing recurrent choledocholithiasis and biliary strictures, with stenting failing to resolve symptoms. Biopsy from a stricture at the lower third of the common bile duct showed focal high-grade dysplasia. A Whipple procedure was aborted intraoperatively after many nodular hepatic lesions were seen. Pathology of these lesions revealed caseating granulomas without malignancy (Figure 1).
An extensive infectious workup showed positive serology for brucella and antibiotic therapy was initiated and continued for five of twelve weeks, improving symptoms and labs. Serial ERCPs revealed an ampullary adenocarcinoma. A Whipple procedure was performed with negative margins, with pathology showing pancreatic invasion with positive lymph nodes. Postoperatively, he improved clinically with serial labs showing a drastic reduction in liver enzymes. He began chemotherapy and completed a course of antibiotics with resolution of his symptoms.
Discussion: Ampullary adenocarcinoma is a rare malignancy that makes up 0.2% of gastrointestinal cancers. It is not known to be associated with chronic infection of the biliary tree or biliary dysplasia.
Biliary involvement in brucellosis is rare, with only limited case reports of acalculous cholecystitis and vanishing bile duct syndrome. We postulate that chronic brucellosis led to chronic inflammation in our patient’s common bile duct with the eventual development of high-grade dysplasia and strictures, potentially leading to his recurrent cholangitis. It is possible that his partial course of antibiotics contributed to the resolution of his obstructive symptoms; however, his symptoms recurred, likely due to incomplete eradication.
There is no known precedent for chronic brucellosis directly contributing to ampullary adenocarcinoma, but due to the high-grade dysplasia in the distal common bile duct and its proximity to the ampulla, it is possible that the cells of the ampulla could have been affected, potentially contributing to the development of the malignancy.
Disclosures:
Zachary C. Vinton, DO1, Kevin Wolfe, DO2, Matthew Stotts, MD, MPH3, Mark Rosenblatt, MD4, Clark Kulig, MD3, Kathy Sotelo, MD3, Thomas Heffron, MD3, Vimal Jhaveri, MD3. P0074 - Chronic Hepatobiliary Brucellosis With the Novel Development of Focal Invasive Ampullary Adenocarcinoma: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Nebraska Medical Center, Omaha, NE; 2Hennepin Healthcare, Minneapolis, MN; 3Presbyterian/St. Luke's Medical Center, Denver, CO; 4UCHealth Longmont, Longmont, CO
Introduction: Brucellosis is a zoonotic bacterial infection with a long and recurrent course of disease. While biliary complications can occur, there are no reported cases of biliary dysplasia or gastrointestinal malignancy associated with brucellosis.
Case Description/Methods: A 68-year-old male with a history of cholecystitis requiring cholecystectomy presented with 18 months of night sweats, headaches, intermittent fevers, muscle wasting, and weight loss. Multiple ERCPs were performed revealing recurrent choledocholithiasis and biliary strictures, with stenting failing to resolve symptoms. Biopsy from a stricture at the lower third of the common bile duct showed focal high-grade dysplasia. A Whipple procedure was aborted intraoperatively after many nodular hepatic lesions were seen. Pathology of these lesions revealed caseating granulomas without malignancy (Figure 1).
An extensive infectious workup showed positive serology for brucella and antibiotic therapy was initiated and continued for five of twelve weeks, improving symptoms and labs. Serial ERCPs revealed an ampullary adenocarcinoma. A Whipple procedure was performed with negative margins, with pathology showing pancreatic invasion with positive lymph nodes. Postoperatively, he improved clinically with serial labs showing a drastic reduction in liver enzymes. He began chemotherapy and completed a course of antibiotics with resolution of his symptoms.
Discussion: Ampullary adenocarcinoma is a rare malignancy that makes up 0.2% of gastrointestinal cancers. It is not known to be associated with chronic infection of the biliary tree or biliary dysplasia.
Biliary involvement in brucellosis is rare, with only limited case reports of acalculous cholecystitis and vanishing bile duct syndrome. We postulate that chronic brucellosis led to chronic inflammation in our patient’s common bile duct with the eventual development of high-grade dysplasia and strictures, potentially leading to his recurrent cholangitis. It is possible that his partial course of antibiotics contributed to the resolution of his obstructive symptoms; however, his symptoms recurred, likely due to incomplete eradication.
There is no known precedent for chronic brucellosis directly contributing to ampullary adenocarcinoma, but due to the high-grade dysplasia in the distal common bile duct and its proximity to the ampulla, it is possible that the cells of the ampulla could have been affected, potentially contributing to the development of the malignancy.
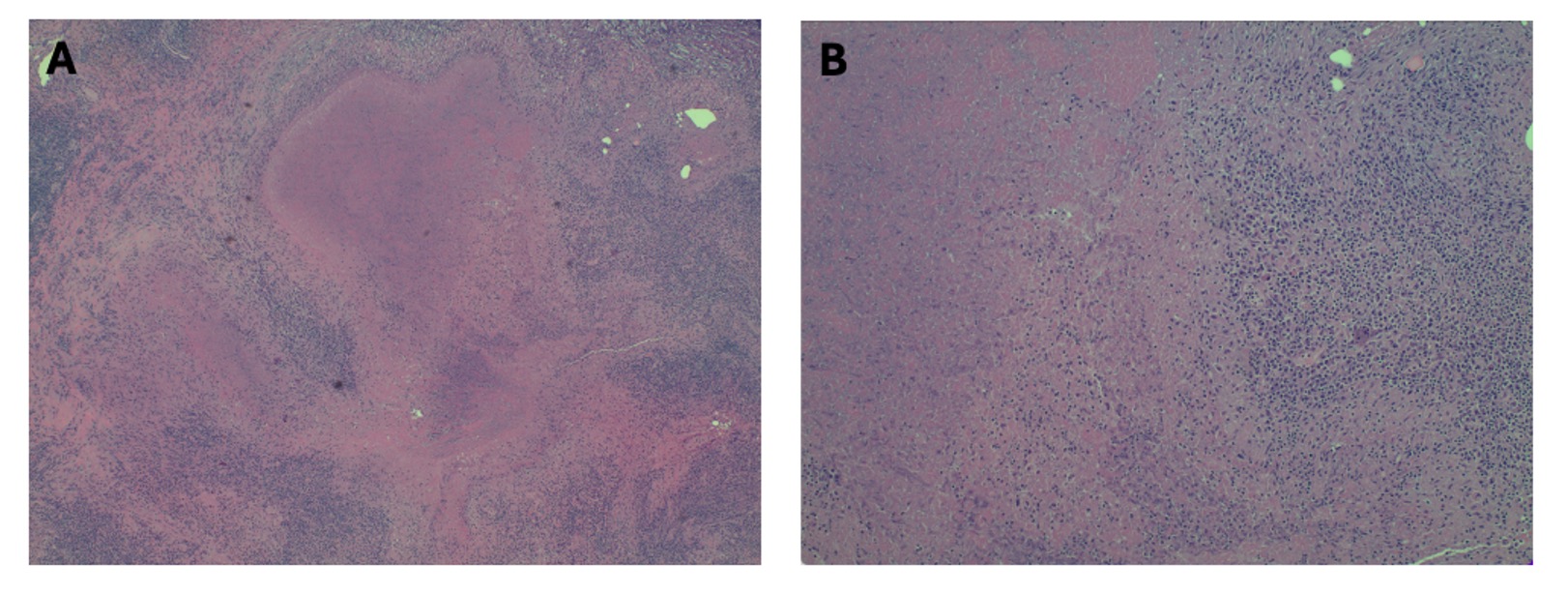
Figure: Figure 1. Surgical pathology slides from nodular hepatic parenchyma
Shown on the left (Figure 1A) is a low-power view showing geographic areas of caseating granulomatous inflammation surrounded by chronic inflammation in the liver. On the right (Figure 2A) is a high-power view showing necrosis on the left and chronic inflammatory infiltrate with mostly plasma cells and lymphocytes on the right.
Shown on the left (Figure 1A) is a low-power view showing geographic areas of caseating granulomatous inflammation surrounded by chronic inflammation in the liver. On the right (Figure 2A) is a high-power view showing necrosis on the left and chronic inflammatory infiltrate with mostly plasma cells and lymphocytes on the right.
Disclosures:
Zachary Vinton indicated no relevant financial relationships.
Kevin Wolfe indicated no relevant financial relationships.
Matthew Stotts indicated no relevant financial relationships.
Mark Rosenblatt indicated no relevant financial relationships.
Clark Kulig indicated no relevant financial relationships.
Kathy Sotelo indicated no relevant financial relationships.
Thomas Heffron indicated no relevant financial relationships.
Vimal Jhaveri indicated no relevant financial relationships.
Zachary C. Vinton, DO1, Kevin Wolfe, DO2, Matthew Stotts, MD, MPH3, Mark Rosenblatt, MD4, Clark Kulig, MD3, Kathy Sotelo, MD3, Thomas Heffron, MD3, Vimal Jhaveri, MD3. P0074 - Chronic Hepatobiliary Brucellosis With the Novel Development of Focal Invasive Ampullary Adenocarcinoma: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
