Sunday Poster Session
Category: Biliary/Pancreas
P0076 - Malignancy vs Infection? A Case of Disseminated Histoplasmosis Presenting as Pancreatic Head Mass
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Cristina Chiodi, MD
University of Louisville School of Medicine
Sarasota, FL
Presenting Author(s)
Cristina Chiodi, MD1, David Liu, MD2, Michael Hogg, MD3, Mikayla Hennen, DO2, Nathan Liu, MD3
1University of Louisville School of Medicine, Sarasota, FL; 2University of Louisville School of Medicine, Louisville, KY; 3University of Louisville, Louisville, KY
Introduction: Histoplasma is endemic to Mississippi and Ohio River Valley regions of the United States. This infection primarily occurs via inhalation of airborne conidia, proliferation within tissue macrophages, and hematogenous or lymphatic spread. While often an asymptomatic pulmonary infection, histoplasmosis can infrequently present as GI disease in immunocompromised patients. We describe a case of disseminated histoplasmosis in AIDS patient, presenting as epigastric pain and unintentional weight loss with pancreatic head mass.
Case Description/Methods: 47 year-old male with history of HIV and histoplasmosis presented for one week of epigastric abdominal pain. One year prior to current presentation, patient was diagnosed with AIDS (CD4 11) and disseminated histoplasmosis when he sought medical attention for generalized malaise, unintentional weight loss, and shortness of breath. CT Chest noted diffuse infiltrates within lungs with hilar adenopathy. CT Abdomen was unremarkable at that time. Patient was started on induction therapy with ART and Amphotericin, then was transitioned to itraconazole for suppressive therapy on discharge. Patient was ultimately lost to follow-up.
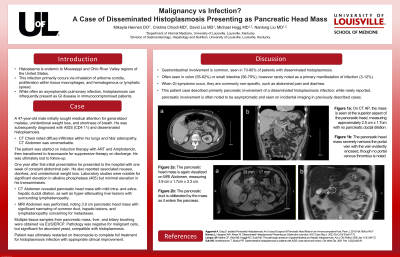
On presentation, he reported one week of constant abdominal pain, with associated nausea, diarrhea, and unintentional weight loss. Laboratory studies were notable for significant elevation in ALP (405) with minimal transaminitis. CT Abdomen revealed pancreatic head mass with intra- and extra-hepatic ductal dilation, as well as hyper-attenuating liver lesions. MRI noted 3.9 cm pancreatic head mass with significant narrowing of common duct, hepatic lesions, and lymphadenopathy concerning for metastases. Multiple tissue samples from pancreatic mass, liver, and biliary brushing were obtained via EUS/ERCP. Pathology was negative for malignant cells, but significant for abundant yeast, compatible with histoplasmosis. Patient was restarted on itraconazole to complete full treatment for histoplasmosis infection with progressive clinical improvement.
Discussion: GI involvement is present in 70-90% of patients with disseminated histoplasmosis. Often seen in colon (55-62%) or small intestine (56-79%), however rarely noted as a primary manifestation of infection (3-12%). When GI symptoms occur, they are commonly non-specific, such as abdominal pain and diarrhea. This patient case described primarily pancreatic involvement; while rarely reported, previously described cases of pancreatic involvement were asymptomatic and seen on incidental imaging.
Disclosures:
Cristina Chiodi, MD1, David Liu, MD2, Michael Hogg, MD3, Mikayla Hennen, DO2, Nathan Liu, MD3. P0076 - Malignancy vs Infection? A Case of Disseminated Histoplasmosis Presenting as Pancreatic Head Mass, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Louisville School of Medicine, Sarasota, FL; 2University of Louisville School of Medicine, Louisville, KY; 3University of Louisville, Louisville, KY
Introduction: Histoplasma is endemic to Mississippi and Ohio River Valley regions of the United States. This infection primarily occurs via inhalation of airborne conidia, proliferation within tissue macrophages, and hematogenous or lymphatic spread. While often an asymptomatic pulmonary infection, histoplasmosis can infrequently present as GI disease in immunocompromised patients. We describe a case of disseminated histoplasmosis in AIDS patient, presenting as epigastric pain and unintentional weight loss with pancreatic head mass.
Case Description/Methods: 47 year-old male with history of HIV and histoplasmosis presented for one week of epigastric abdominal pain. One year prior to current presentation, patient was diagnosed with AIDS (CD4 11) and disseminated histoplasmosis when he sought medical attention for generalized malaise, unintentional weight loss, and shortness of breath. CT Chest noted diffuse infiltrates within lungs with hilar adenopathy. CT Abdomen was unremarkable at that time. Patient was started on induction therapy with ART and Amphotericin, then was transitioned to itraconazole for suppressive therapy on discharge. Patient was ultimately lost to follow-up.
On presentation, he reported one week of constant abdominal pain, with associated nausea, diarrhea, and unintentional weight loss. Laboratory studies were notable for significant elevation in ALP (405) with minimal transaminitis. CT Abdomen revealed pancreatic head mass with intra- and extra-hepatic ductal dilation, as well as hyper-attenuating liver lesions. MRI noted 3.9 cm pancreatic head mass with significant narrowing of common duct, hepatic lesions, and lymphadenopathy concerning for metastases. Multiple tissue samples from pancreatic mass, liver, and biliary brushing were obtained via EUS/ERCP. Pathology was negative for malignant cells, but significant for abundant yeast, compatible with histoplasmosis. Patient was restarted on itraconazole to complete full treatment for histoplasmosis infection with progressive clinical improvement.
Discussion: GI involvement is present in 70-90% of patients with disseminated histoplasmosis. Often seen in colon (55-62%) or small intestine (56-79%), however rarely noted as a primary manifestation of infection (3-12%). When GI symptoms occur, they are commonly non-specific, such as abdominal pain and diarrhea. This patient case described primarily pancreatic involvement; while rarely reported, previously described cases of pancreatic involvement were asymptomatic and seen on incidental imaging.
Disclosures:
Cristina Chiodi indicated no relevant financial relationships.
David Liu indicated no relevant financial relationships.
Michael Hogg indicated no relevant financial relationships.
Mikayla Hennen indicated no relevant financial relationships.
Nathan Liu indicated no relevant financial relationships.
Cristina Chiodi, MD1, David Liu, MD2, Michael Hogg, MD3, Mikayla Hennen, DO2, Nathan Liu, MD3. P0076 - Malignancy vs Infection? A Case of Disseminated Histoplasmosis Presenting as Pancreatic Head Mass, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

