Sunday Poster Session
Category: Biliary/Pancreas
P0079 - Chylothorax and Chylous Ascites: A Rare Complication of Severe Acute Necrotizing Pancreatitis and Direct Endoscopic Necrosectomy (DEN)
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- UG
Udita Gupta, MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Udita Gupta, MD1, Parth Patel, MD1, Supriya Maheshwari, MBBS1, Abhinav Vyas, MD2, Sergio A. Sánchez-Luna, MD3
1University of Alabama at Birmingham, Birmingham, AL; 2Vanderbilt University Medical Center, Nashville, TN; 3Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Chylothorax is typically caused by traumatic injury, obstruction, infection, or malignancy. Chylous ascites can be caused by similar mechanisms, including necrotizing pancreatitis.
Case Description/Methods: A 73-year-old male was admitted with a diagnosis of acute biliary pancreatitis for which he underwent cholecystectomy. He developed severe necrotizing pancreatitis with WON formation. Initial imaging was negative for any peritoneal or pleural fluid collections. He then underwent EUS-guided drainage and direct endoscopic necrosectomy (DEN) using a lumen-apposing metal stent (LAMS).
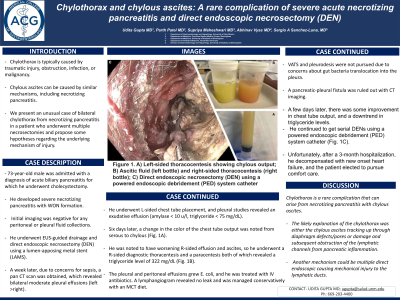
A week later, due to concerns for sepsis, a pan CT scan was obtained, which revealed bilateral moderate pleural effusions (left >right). He underwent L-sided chest tube placement, and pleural studies revealed an exudative effusion (amylase < 10 u/l, triglyceride < 75 mg/dL). Six days later, a change in the color of the chest tube output was noted from serous to chylous (Fig. 1A). He was noted to have worsening R-sided effusion and ascites, so he underwent a R-sided diagnostic thoracentesis and a paracentesis both of which revealed a triglyceride level of 322 mg/dL (Fig. 1B). The pleural and peritoneal effusions grew E. coli, and he was treated with IV antibiotics. A lymphangiogram revealed no leak and was managed conservatively with an MCT diet. VATS and pleurodesis were not pursued due to concerns about gut bacteria translocation into the pleura. A pancreatic-pleural fistula was ruled out with CT imaging. A few days later, there was some improvement in chest tube output, and a downtrend in triglyceride levels. He continued to get serial DENs using a powered endoscopic debridement (PED) system catheter (Fig. 1C). Unfortunately, after a 3-month hospitalization, he decompensated with new onset heart failure, and the patient elected to pursue comfort care.
Discussion: Chylothorax is a rare complication that can arise from necrotizing pancreatitis with chylous ascites. The likely explanation of the chylothorax was either the chylous ascites tracking up through diaphragm defects/pores or damage and subsequent obstruction of the lymphatic channels from pancreatic inflammation. Another mechanism could be multiple direct endoscopic causing mechanical injury to the lymphatic ducts. In summary, we present an unusual case of bilateral chylothorax from necrotizing pancreatitis in a patient who underwent multiple necrosectomies and propose some hypotheses regarding the underlying mechanism of injury.

Disclosures:
Udita Gupta, MD1, Parth Patel, MD1, Supriya Maheshwari, MBBS1, Abhinav Vyas, MD2, Sergio A. Sánchez-Luna, MD3. P0079 - Chylothorax and Chylous Ascites: A Rare Complication of Severe Acute Necrotizing Pancreatitis and Direct Endoscopic Necrosectomy (DEN), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham, Birmingham, AL; 2Vanderbilt University Medical Center, Nashville, TN; 3Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Chylothorax is typically caused by traumatic injury, obstruction, infection, or malignancy. Chylous ascites can be caused by similar mechanisms, including necrotizing pancreatitis.
Case Description/Methods: A 73-year-old male was admitted with a diagnosis of acute biliary pancreatitis for which he underwent cholecystectomy. He developed severe necrotizing pancreatitis with WON formation. Initial imaging was negative for any peritoneal or pleural fluid collections. He then underwent EUS-guided drainage and direct endoscopic necrosectomy (DEN) using a lumen-apposing metal stent (LAMS).
A week later, due to concerns for sepsis, a pan CT scan was obtained, which revealed bilateral moderate pleural effusions (left >right). He underwent L-sided chest tube placement, and pleural studies revealed an exudative effusion (amylase < 10 u/l, triglyceride < 75 mg/dL). Six days later, a change in the color of the chest tube output was noted from serous to chylous (Fig. 1A). He was noted to have worsening R-sided effusion and ascites, so he underwent a R-sided diagnostic thoracentesis and a paracentesis both of which revealed a triglyceride level of 322 mg/dL (Fig. 1B). The pleural and peritoneal effusions grew E. coli, and he was treated with IV antibiotics. A lymphangiogram revealed no leak and was managed conservatively with an MCT diet. VATS and pleurodesis were not pursued due to concerns about gut bacteria translocation into the pleura. A pancreatic-pleural fistula was ruled out with CT imaging. A few days later, there was some improvement in chest tube output, and a downtrend in triglyceride levels. He continued to get serial DENs using a powered endoscopic debridement (PED) system catheter (Fig. 1C). Unfortunately, after a 3-month hospitalization, he decompensated with new onset heart failure, and the patient elected to pursue comfort care.
Discussion: Chylothorax is a rare complication that can arise from necrotizing pancreatitis with chylous ascites. The likely explanation of the chylothorax was either the chylous ascites tracking up through diaphragm defects/pores or damage and subsequent obstruction of the lymphatic channels from pancreatic inflammation. Another mechanism could be multiple direct endoscopic causing mechanical injury to the lymphatic ducts. In summary, we present an unusual case of bilateral chylothorax from necrotizing pancreatitis in a patient who underwent multiple necrosectomies and propose some hypotheses regarding the underlying mechanism of injury.

Figure: Figure 1. A) Left-sided thoracocentesis showing chylous output; B) Ascitic fluid (left bottle) and right-sided thoracocentesis (right bottle); C) Direct endoscopic necrosectomy (DEN) using a powered endoscopic debridement (PED) system catheter.
Disclosures:
Udita Gupta indicated no relevant financial relationships.
Parth Patel indicated no relevant financial relationships.
Supriya Maheshwari indicated no relevant financial relationships.
Abhinav Vyas indicated no relevant financial relationships.
Sergio A. Sánchez-Luna indicated no relevant financial relationships.
Udita Gupta, MD1, Parth Patel, MD1, Supriya Maheshwari, MBBS1, Abhinav Vyas, MD2, Sergio A. Sánchez-Luna, MD3. P0079 - Chylothorax and Chylous Ascites: A Rare Complication of Severe Acute Necrotizing Pancreatitis and Direct Endoscopic Necrosectomy (DEN), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
