Sunday Poster Session
Category: Biliary/Pancreas
P0080 - When Nature Imitates Science: Hemorrhagic Pancreatic Pseudocyst Within a Naturally Occurring Cyst-Gastrostomy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Hannah Fiske, MD
Brown University / Rhode Island Hospital
Providence, RI
Presenting Author(s)
Hannah Fiske, MD1, Daniel Marino, MD, MBA2, Harlan Rich, MD1
1Brown University / Rhode Island Hospital, Providence, RI; 2NYU Langone Health, New York, NY
Introduction: Pancreatic pseudocysts are encapsulated fluid collections which occur in ~30% of patients with chronic pancreatitis. Symptomatic pseudocysts may be treated via endoscopic cyst-gastrostomy, where a communication is made between pseudocyst and stomach, allowing for drainage into the GI tract and avoiding the need for an external drain. If the pseudocyst erodes through a blood vessel wall it can cause hemorrhage, a rare complication with often catastrophic consequences requiring immediate intervention.
Case Description/Methods: Our patient is a 45yo male with chronic pancreatitis complicated by splenic vein thrombosis and left sided portal HTN. He presented with hematochezia, anorexia, emesis, and a non-tender enlarging RUQ mass. Hgb on admission was 5.8mg/dL (baseline 13), improving appropriately to ~8 with transfusion of 2U pRBC. EGD showed erosive esophagitis and an area in the proximal gastric lumen resembling a cyst-gastrostomy.
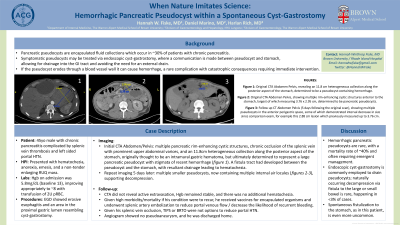
Imaging revealed multiple pancreatic rim-enhancing cystic structures, chronic occlusion of the splenic vein with prominent upper abdominal varices, and an 11.8cm heterogeneous collection along the posterior aspect of the stomach, originally thought to be an intramural gastric hematoma, but ultimately determined to represent a large pancreatic pseudocyst with stigmata of recent hemorrhage (image 1a). A fistula tract had developed between the pseudocyst and the stomach, with resultant drainage likely leading to hematochezia.
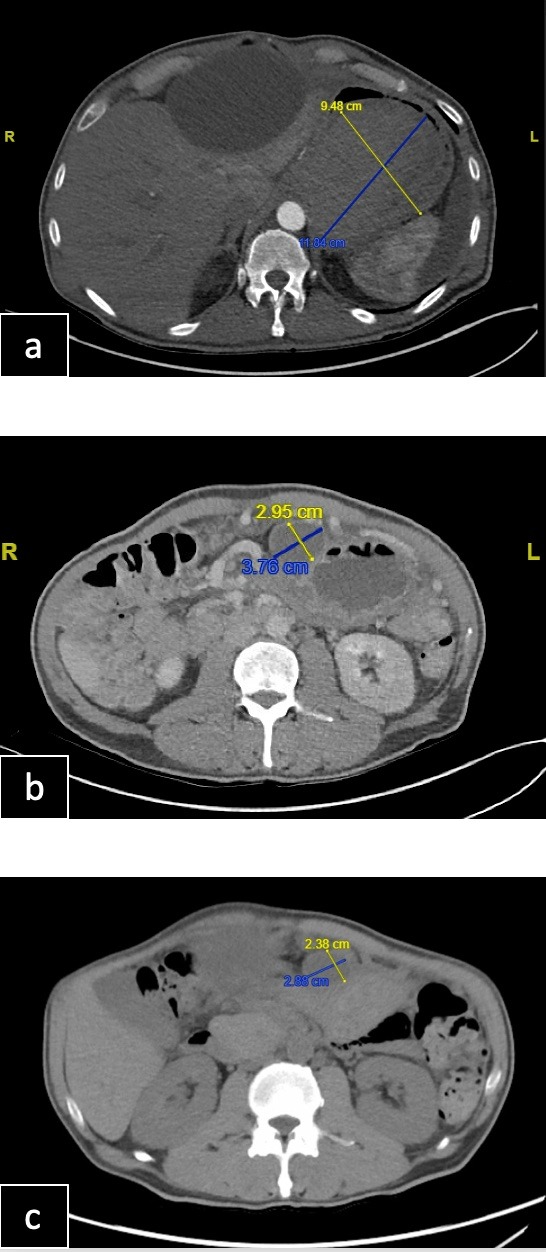
Repeat imaging 5 days later revealed multiple pseudocysts of decreased size, now containing multiple internal air locules (image 1b-c), supporting decompression. CTA did not reveal active extravasation, Hgb remained stable, and there was no additional hematochezia. Given high morbidity/mortality if his condition were to recur, he received vaccines for encapsulated organisms and underwent splenic artery embolization to reduce portal venous flow and decrease the likelihood of recurrent bleeding. Given his splenic vein occlusion, TIPS or BRTO were not options to reduce portal HTN. Angiogram showed no pseudoaneurysm, and he was discharged home.
Discussion: Hemorrhagic pancreatic pseudocysts are rare, with a mortality rate of ~40% and often requiring emergent management. Endoscopic cyst-gastrostomy is commonly employed to drain pseudocysts; spontaneous decompression via fistula to the large or small bowel is rare, occurring in fewer than 3% of cases. Spontaneous fistulization to the stomach, as in this patient, is even more uncommon.
Disclosures:
Hannah Fiske, MD1, Daniel Marino, MD, MBA2, Harlan Rich, MD1. P0080 - When Nature Imitates Science: Hemorrhagic Pancreatic Pseudocyst Within a Naturally Occurring Cyst-Gastrostomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown University / Rhode Island Hospital, Providence, RI; 2NYU Langone Health, New York, NY
Introduction: Pancreatic pseudocysts are encapsulated fluid collections which occur in ~30% of patients with chronic pancreatitis. Symptomatic pseudocysts may be treated via endoscopic cyst-gastrostomy, where a communication is made between pseudocyst and stomach, allowing for drainage into the GI tract and avoiding the need for an external drain. If the pseudocyst erodes through a blood vessel wall it can cause hemorrhage, a rare complication with often catastrophic consequences requiring immediate intervention.
Case Description/Methods: Our patient is a 45yo male with chronic pancreatitis complicated by splenic vein thrombosis and left sided portal HTN. He presented with hematochezia, anorexia, emesis, and a non-tender enlarging RUQ mass. Hgb on admission was 5.8mg/dL (baseline 13), improving appropriately to ~8 with transfusion of 2U pRBC. EGD showed erosive esophagitis and an area in the proximal gastric lumen resembling a cyst-gastrostomy.
Imaging revealed multiple pancreatic rim-enhancing cystic structures, chronic occlusion of the splenic vein with prominent upper abdominal varices, and an 11.8cm heterogeneous collection along the posterior aspect of the stomach, originally thought to be an intramural gastric hematoma, but ultimately determined to represent a large pancreatic pseudocyst with stigmata of recent hemorrhage (image 1a). A fistula tract had developed between the pseudocyst and the stomach, with resultant drainage likely leading to hematochezia.
Repeat imaging 5 days later revealed multiple pseudocysts of decreased size, now containing multiple internal air locules (image 1b-c), supporting decompression. CTA did not reveal active extravasation, Hgb remained stable, and there was no additional hematochezia. Given high morbidity/mortality if his condition were to recur, he received vaccines for encapsulated organisms and underwent splenic artery embolization to reduce portal venous flow and decrease the likelihood of recurrent bleeding. Given his splenic vein occlusion, TIPS or BRTO were not options to reduce portal HTN. Angiogram showed no pseudoaneurysm, and he was discharged home.
Discussion: Hemorrhagic pancreatic pseudocysts are rare, with a mortality rate of ~40% and often requiring emergent management. Endoscopic cyst-gastrostomy is commonly employed to drain pseudocysts; spontaneous decompression via fistula to the large or small bowel is rare, occurring in fewer than 3% of cases. Spontaneous fistulization to the stomach, as in this patient, is even more uncommon.
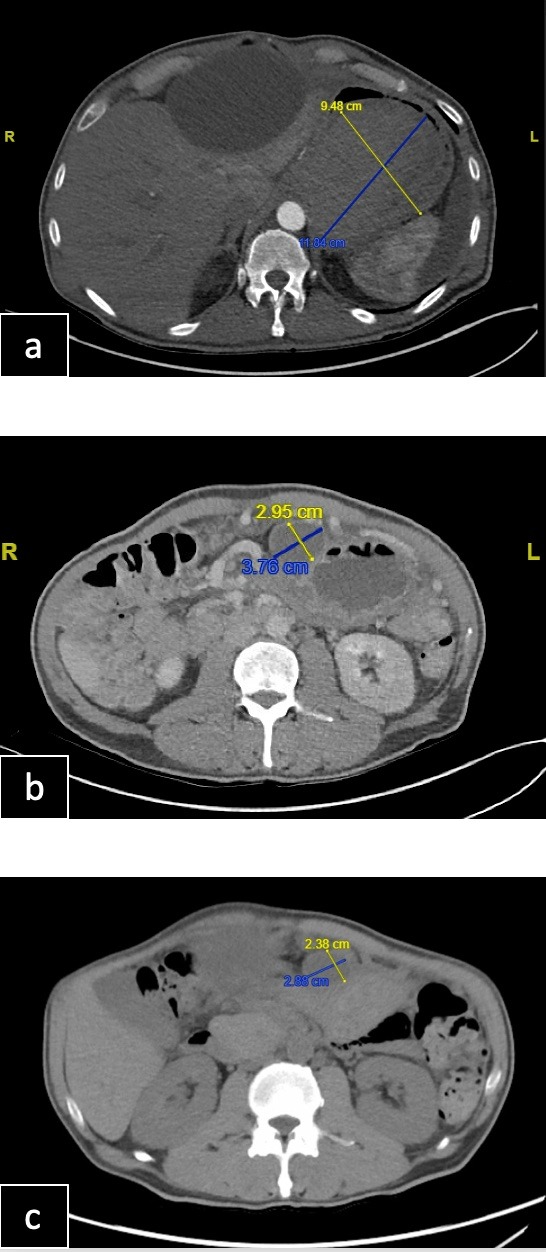
Figure: Image 1.
a) Original CTA Abdomen Pelvis, revealing an 11.8 cm heterogeneous collection along the posterior aspect of the stomach, determined to be a pseudocyst-containing hemorrhage.
b) Original CTA Abdomen Pelvis, showing multiple rim-enhancing cystic structures anterior to the stomach, largest of which measuring 3.76 x 2.95 cm, determined to be pancreatic pseudocysts.
c) Follow up CT Abdomen Pelvis (5 days following the original scan), showing multiple pseudocysts in the anterior perigastric space, some of which demonstrated interval decrease in size since comparison exam, for example this 2.88 cm lesion which previously measured up to 3.76 cm.
a) Original CTA Abdomen Pelvis, revealing an 11.8 cm heterogeneous collection along the posterior aspect of the stomach, determined to be a pseudocyst-containing hemorrhage.
b) Original CTA Abdomen Pelvis, showing multiple rim-enhancing cystic structures anterior to the stomach, largest of which measuring 3.76 x 2.95 cm, determined to be pancreatic pseudocysts.
c) Follow up CT Abdomen Pelvis (5 days following the original scan), showing multiple pseudocysts in the anterior perigastric space, some of which demonstrated interval decrease in size since comparison exam, for example this 2.88 cm lesion which previously measured up to 3.76 cm.
Disclosures:
Hannah Fiske indicated no relevant financial relationships.
Daniel Marino indicated no relevant financial relationships.
Harlan Rich indicated no relevant financial relationships.
Hannah Fiske, MD1, Daniel Marino, MD, MBA2, Harlan Rich, MD1. P0080 - When Nature Imitates Science: Hemorrhagic Pancreatic Pseudocyst Within a Naturally Occurring Cyst-Gastrostomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
