Sunday Poster Session
Category: Biliary/Pancreas
P0089 - Lemmel Syndrome: An Unusual Cause of Biliary Obstruction
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Leith Ghani, DO
Banner University Medical Center
Paradise Valley, AZ
Presenting Author(s)
Leith Ghani, DO1, Kyle Pierce, DO2, Elizabeth Rowland, MD3, Kaivan Salehpour, MD4, Hugo Pinillos, MD, FACG5
1Banner University Medical Center, Phoenix, AZ; 2University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ; 3University of Arizona College of Medicine, Phoenix, AZ; 4Phoenix VA Health Care System, La Verne, CA; 5Carl T. Hayden Veterans' Administration Medical Center, Phoenix, AZ
Introduction: Lemmel syndrome is a rare condition that causes obstructive jaundice due to a periampullary duodenal diverticulum compressing the common bile duct (CBD) or pancreatic duct. It is identifiable by the absence of choledocholithiasis or pancreaticobiliary tumors. Its prevalence is poorly documented because of its rarity and frequent misdiagnosis as other conditions like pancreatic head tumors. Lemmel syndrome is typically discovered incidentally during imaging for other conditions due to its lack of specific signs and underreporting. The syndrome’s diagnosis relies on imaging, with Magnetic Resonance Cholangiopancreatography (MRCP) being preferred for its non-invasive nature and sensitivity. However, Endoscopic Retrograde Cholangiopancreatography (ERCP) is the gold standard for both diagnosis and treatment because of its capacity for direct visualization and intervention.
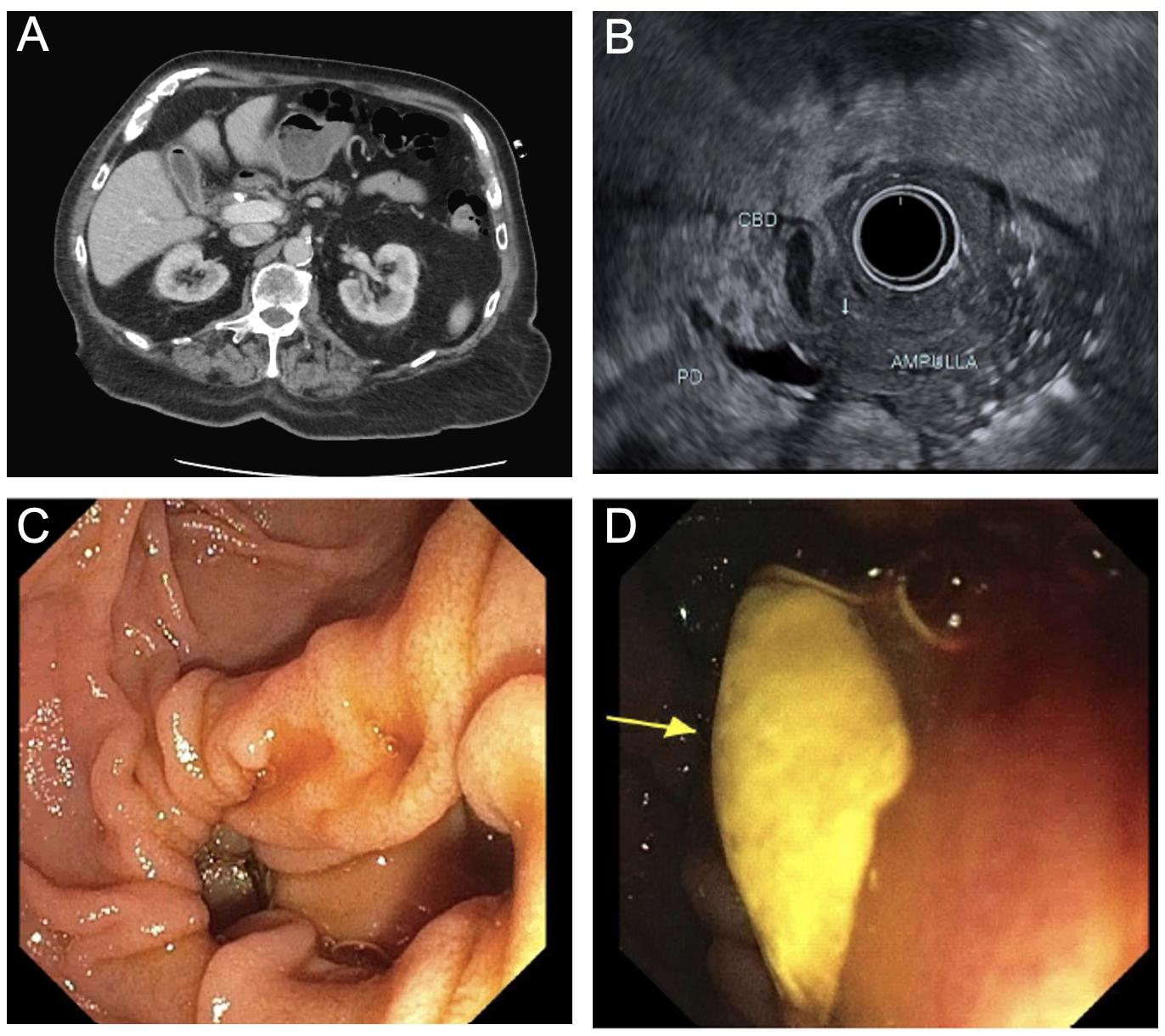
Case Description/Methods: An 83-year-old male presented with one day of fever, chills, nausea, and vomiting. Labs showed a cholestatic injury with total bilirubin 4.9, AST 270, ALT 70, and ALP 256. Blood cultures revealed Klebsiella oxytoca. Initial CT abdomen was notable for pericholecystic fluid collection and gas in the gallbladder lumen.
With concerns for ascending cholangitis, he underwent an urgent ERCP. Upon entering the duodenum, an adjacent periampullary diverticulum filled with green and white thickened fluid was noted (Figure 1). There was marked angulation of the CBD at the ampulla with the periampullary diverticulum, suggesting extrinsic compression. The ampulla, located within the diverticular cavity, was difficult to access. A balloon sweep was successfully completed with sludge extraction, and a plastic biliary stent was placed. Significant additional purulent material was removed from the ampulla. A follow-up HIDA scan one month later showed no evidence of acute or chronic cholecystitis and the passage of the biliary stent.
Discussion: This case underscores the importance of considering Lemmel syndrome in patients with obstructive jaundice, particularly when initial imaging does not reveal common etiologies such as choledocholithiasis or pancreaticobiliary tumors. Accurate diagnosis hinges on advanced imaging modalities, and endoscopic management plays a vital role in alleviating symptoms and improving patient outcomes. Increased awareness and reporting of Lemmel syndrome are essential for enhancing understanding and management of this rare but significant condition.
Disclosures:
Leith Ghani, DO1, Kyle Pierce, DO2, Elizabeth Rowland, MD3, Kaivan Salehpour, MD4, Hugo Pinillos, MD, FACG5. P0089 - Lemmel Syndrome: An Unusual Cause of Biliary Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Banner University Medical Center, Phoenix, AZ; 2University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ; 3University of Arizona College of Medicine, Phoenix, AZ; 4Phoenix VA Health Care System, La Verne, CA; 5Carl T. Hayden Veterans' Administration Medical Center, Phoenix, AZ
Introduction: Lemmel syndrome is a rare condition that causes obstructive jaundice due to a periampullary duodenal diverticulum compressing the common bile duct (CBD) or pancreatic duct. It is identifiable by the absence of choledocholithiasis or pancreaticobiliary tumors. Its prevalence is poorly documented because of its rarity and frequent misdiagnosis as other conditions like pancreatic head tumors. Lemmel syndrome is typically discovered incidentally during imaging for other conditions due to its lack of specific signs and underreporting. The syndrome’s diagnosis relies on imaging, with Magnetic Resonance Cholangiopancreatography (MRCP) being preferred for its non-invasive nature and sensitivity. However, Endoscopic Retrograde Cholangiopancreatography (ERCP) is the gold standard for both diagnosis and treatment because of its capacity for direct visualization and intervention.
Case Description/Methods: An 83-year-old male presented with one day of fever, chills, nausea, and vomiting. Labs showed a cholestatic injury with total bilirubin 4.9, AST 270, ALT 70, and ALP 256. Blood cultures revealed Klebsiella oxytoca. Initial CT abdomen was notable for pericholecystic fluid collection and gas in the gallbladder lumen.
With concerns for ascending cholangitis, he underwent an urgent ERCP. Upon entering the duodenum, an adjacent periampullary diverticulum filled with green and white thickened fluid was noted (Figure 1). There was marked angulation of the CBD at the ampulla with the periampullary diverticulum, suggesting extrinsic compression. The ampulla, located within the diverticular cavity, was difficult to access. A balloon sweep was successfully completed with sludge extraction, and a plastic biliary stent was placed. Significant additional purulent material was removed from the ampulla. A follow-up HIDA scan one month later showed no evidence of acute or chronic cholecystitis and the passage of the biliary stent.
Discussion: This case underscores the importance of considering Lemmel syndrome in patients with obstructive jaundice, particularly when initial imaging does not reveal common etiologies such as choledocholithiasis or pancreaticobiliary tumors. Accurate diagnosis hinges on advanced imaging modalities, and endoscopic management plays a vital role in alleviating symptoms and improving patient outcomes. Increased awareness and reporting of Lemmel syndrome are essential for enhancing understanding and management of this rare but significant condition.
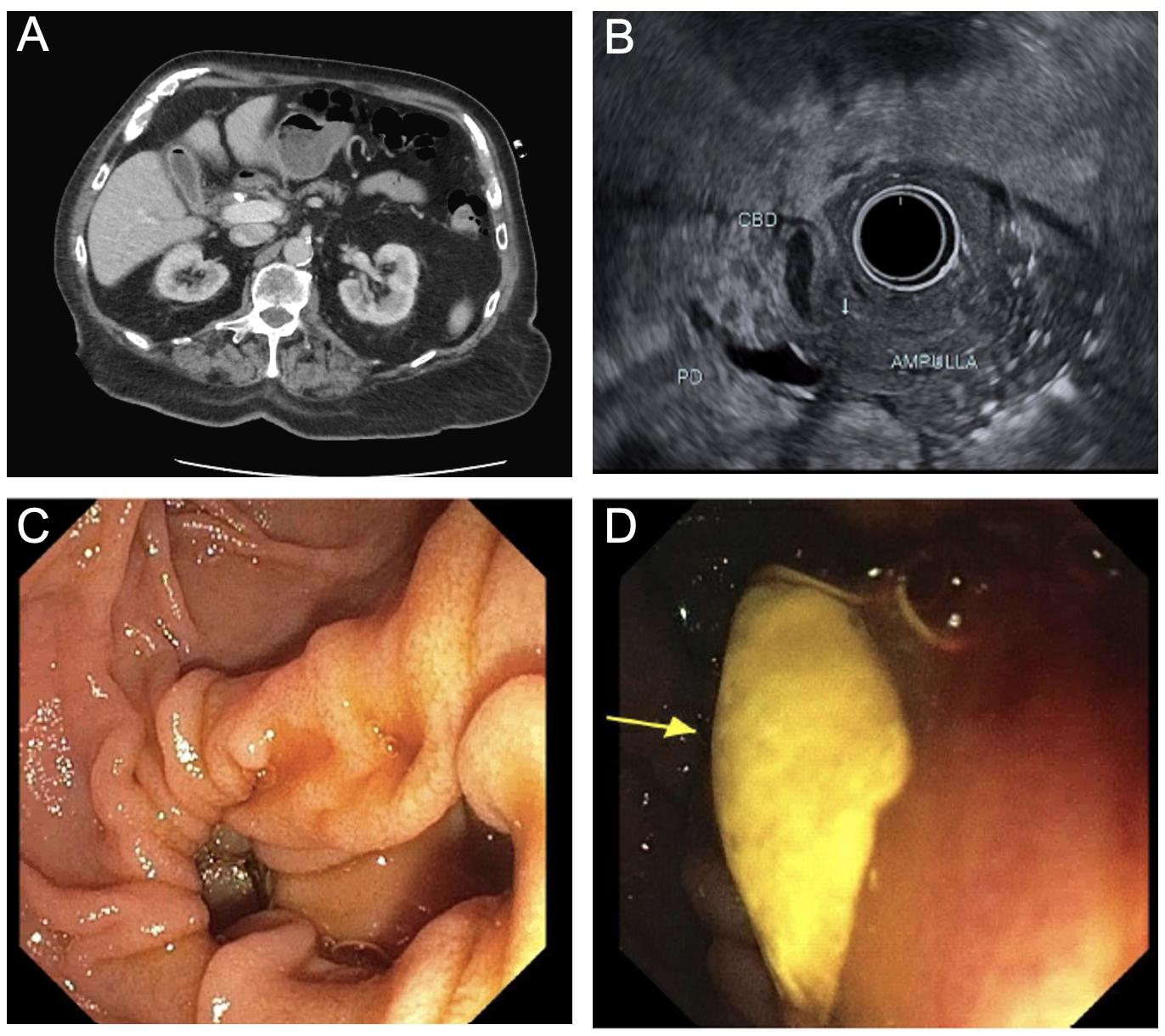
Figure: Figure 1: A: Axial view on CT scan revealing pericholecystic fluid collection and gas in the gallbladder lumen. B: Endoscopic ultrasound revealing periampullary duodenal diverticulum in the 2nd portion of the duodenum with diverticulum and localized edema around papilla. C: Endoscopy exhibiting marked angulation of the CBD at the ampulla with the periampullary diverticulum D: Endoscopy revealing periampullary diverticulum filled with green and white thickened fluid.
Disclosures:
Leith Ghani indicated no relevant financial relationships.
Kyle Pierce indicated no relevant financial relationships.
Elizabeth Rowland indicated no relevant financial relationships.
Kaivan Salehpour indicated no relevant financial relationships.
Hugo Pinillos indicated no relevant financial relationships.
Leith Ghani, DO1, Kyle Pierce, DO2, Elizabeth Rowland, MD3, Kaivan Salehpour, MD4, Hugo Pinillos, MD, FACG5. P0089 - Lemmel Syndrome: An Unusual Cause of Biliary Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
