Sunday Poster Session
Category: Biliary/Pancreas
P0021 - Investigation of Geospatial Disparities in Chronic Pancreatitis Outcomes
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Tamara F. Kahan, MD, MPA
Beth Israel Deaconess Medical Center
Boston, MA
Presenting Author(s)
Tamara Kahan, MD, MPA, Marco Noriega, MD, MPH, Anabel Liyen-Cartelle, MD, Shaharyar Zuberi, MD, Kelsey Anderson, MD, Ankit Chhoda, MBBS, Sunil Sheth, MD
Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Chronic pancreatitis (CP) is a fibro-inflammatory disorder characterized by abdominal pain and exocrine and endocrine pancreatic insufficiency resulting in significant morbidity. This study evaluates the impact of geospatial parameters, assessed using the Social Vulnerability Index (SVI), a tool comprising sixteen social attributes, on CP outcomes, including opioid use.
Methods: We conducted a retrospective analysis of CP patients with available addresses followed at our pancreas center. We reviewed demographics, clinical variables including number of CP flares, local complications, pancreatic function, and healthcare-resource utilization (HRU) including imaging, endoscopic procedures, and surgeries, and outpatient opioid prescriptions measured in morphine milligram equivalents (MME). Regression analysis was performed to assess the association between outcomes and SVI [divided into 4 quartiles (I-IV; IV being most vulnerable].
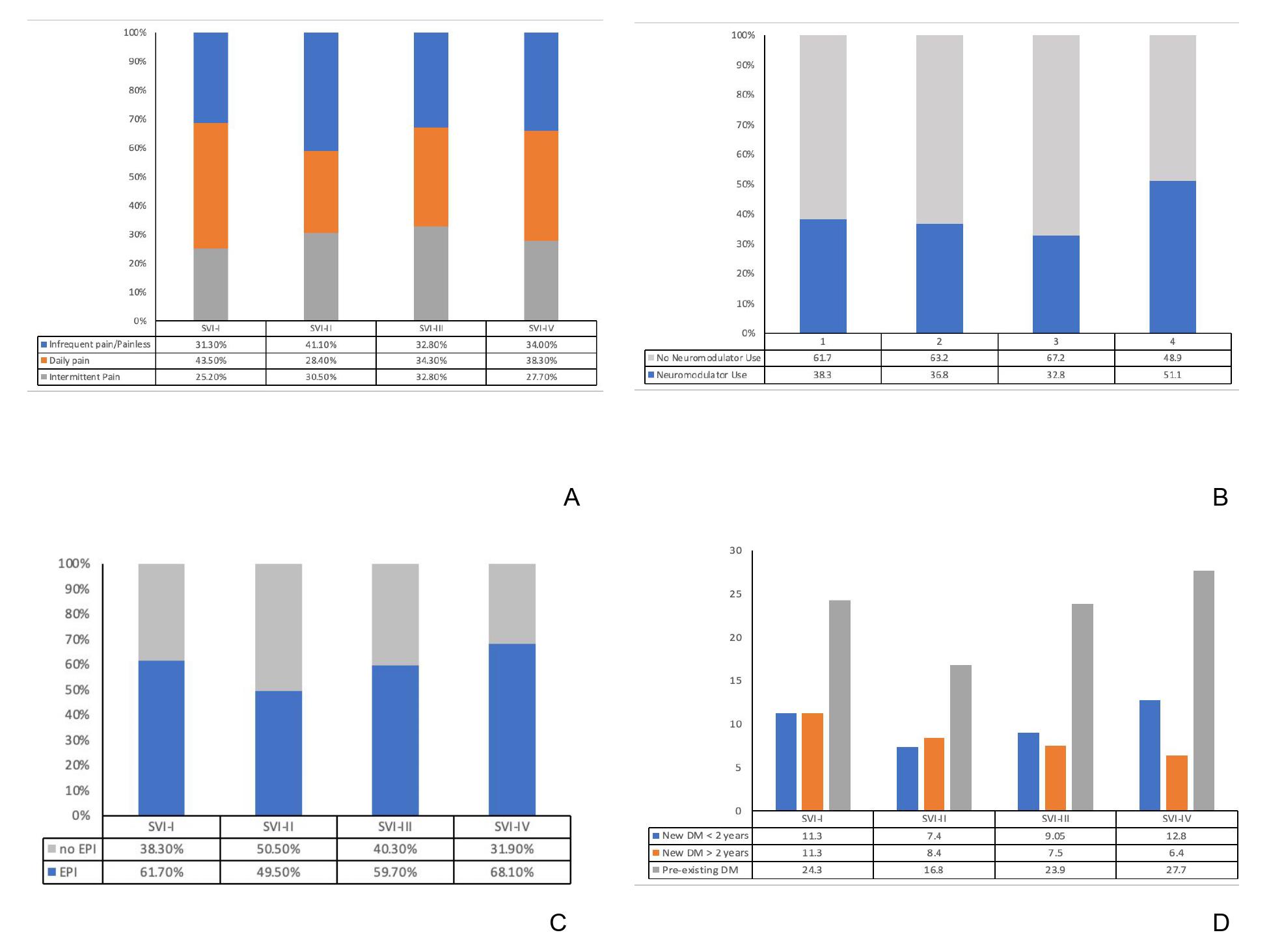
Results: Among 324 CP patients followed over 8 years, we noted trends of higher dependence on governmental insurance or no insurance among patients in higher SVI quartiles (III/IV vs. I/II) but no differences in demographics, comorbidities, or etiology of CP. In patients residing in more vulnerable SVI quartiles, we noted significantly higher frequency of hospitalizations for CP flares and lower daily MME (p< 0.05). Rates of exocrine and endocrine pancreatic dysfunction and HRU were similar across all SVI quartiles (Table 1, Figure 1).
Discussion: Despite multidisciplinary guideline-based care, residence in the most vulnerable neighborhoods was associated with less opioid use and more frequent CP flares, suggesting possible inadequate pain control in these patients. These findings should guide prospective investigation of the impact of geospatial social determinants of health in CP and efforts to mitigate the above disparities.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tamara Kahan, MD, MPA, Marco Noriega, MD, MPH, Anabel Liyen-Cartelle, MD, Shaharyar Zuberi, MD, Kelsey Anderson, MD, Ankit Chhoda, MBBS, Sunil Sheth, MD. P0021 - Investigation of Geospatial Disparities in Chronic Pancreatitis Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Chronic pancreatitis (CP) is a fibro-inflammatory disorder characterized by abdominal pain and exocrine and endocrine pancreatic insufficiency resulting in significant morbidity. This study evaluates the impact of geospatial parameters, assessed using the Social Vulnerability Index (SVI), a tool comprising sixteen social attributes, on CP outcomes, including opioid use.
Methods: We conducted a retrospective analysis of CP patients with available addresses followed at our pancreas center. We reviewed demographics, clinical variables including number of CP flares, local complications, pancreatic function, and healthcare-resource utilization (HRU) including imaging, endoscopic procedures, and surgeries, and outpatient opioid prescriptions measured in morphine milligram equivalents (MME). Regression analysis was performed to assess the association between outcomes and SVI [divided into 4 quartiles (I-IV; IV being most vulnerable].
Results: Among 324 CP patients followed over 8 years, we noted trends of higher dependence on governmental insurance or no insurance among patients in higher SVI quartiles (III/IV vs. I/II) but no differences in demographics, comorbidities, or etiology of CP. In patients residing in more vulnerable SVI quartiles, we noted significantly higher frequency of hospitalizations for CP flares and lower daily MME (p< 0.05). Rates of exocrine and endocrine pancreatic dysfunction and HRU were similar across all SVI quartiles (Table 1, Figure 1).
Discussion: Despite multidisciplinary guideline-based care, residence in the most vulnerable neighborhoods was associated with less opioid use and more frequent CP flares, suggesting possible inadequate pain control in these patients. These findings should guide prospective investigation of the impact of geospatial social determinants of health in CP and efforts to mitigate the above disparities.
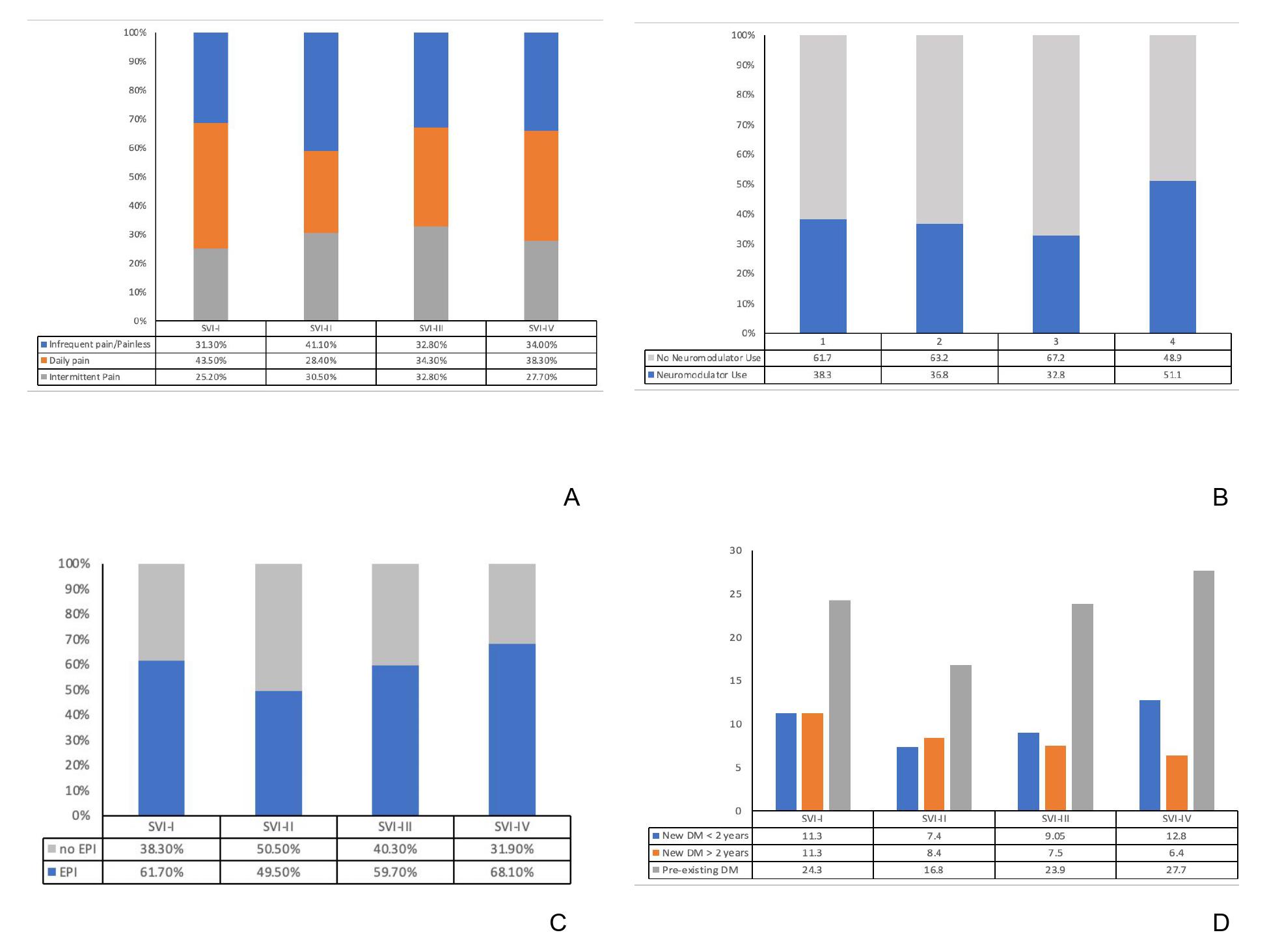
Figure: Frequency distribution among patients with CP describing (A) intermittent, daily abdominal pain, and infrequent pain/painless, (B) neuromodulator use, (C) exocrine pancreatic insufficiency, (D) new onset diabetes mellitus, based on residence in areas across various SVI quartiles.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Tamara Kahan indicated no relevant financial relationships.
Marco Noriega indicated no relevant financial relationships.
Anabel Liyen-Cartelle indicated no relevant financial relationships.
Shaharyar Zuberi indicated no relevant financial relationships.
Kelsey Anderson indicated no relevant financial relationships.
Ankit Chhoda indicated no relevant financial relationships.
Sunil Sheth indicated no relevant financial relationships.
Tamara Kahan, MD, MPA, Marco Noriega, MD, MPH, Anabel Liyen-Cartelle, MD, Shaharyar Zuberi, MD, Kelsey Anderson, MD, Ankit Chhoda, MBBS, Sunil Sheth, MD. P0021 - Investigation of Geospatial Disparities in Chronic Pancreatitis Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

