Sunday Poster Session
Category: Biliary/Pancreas
P0024 - The Influence of Health Disparities and Length of Hospital Stay on 30-Day Readmission Rates in ERCP Patients: A Retrospective Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
- RR
Rajmohan Rammohan, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA
Nassau University Medical Center, East Meadow, NY
Introduction: Hospital readmissions, especially for ERCP patients, reflect care quality and outcomes. ERCP, vital yet risky, can lead to complications necessitating readmission. Comorbidities like diabetes and hypertension, along with LOS, play critical roles. Longer stays may exacerbate complications, while shorter stays risk inadequate recovery. Optimizing LOS balancing acute care needs and risks is crucial. Tailored post-discharge plans and multidisciplinary approaches can mitigate readmission risks, enhancing ERCP patient outcomes.
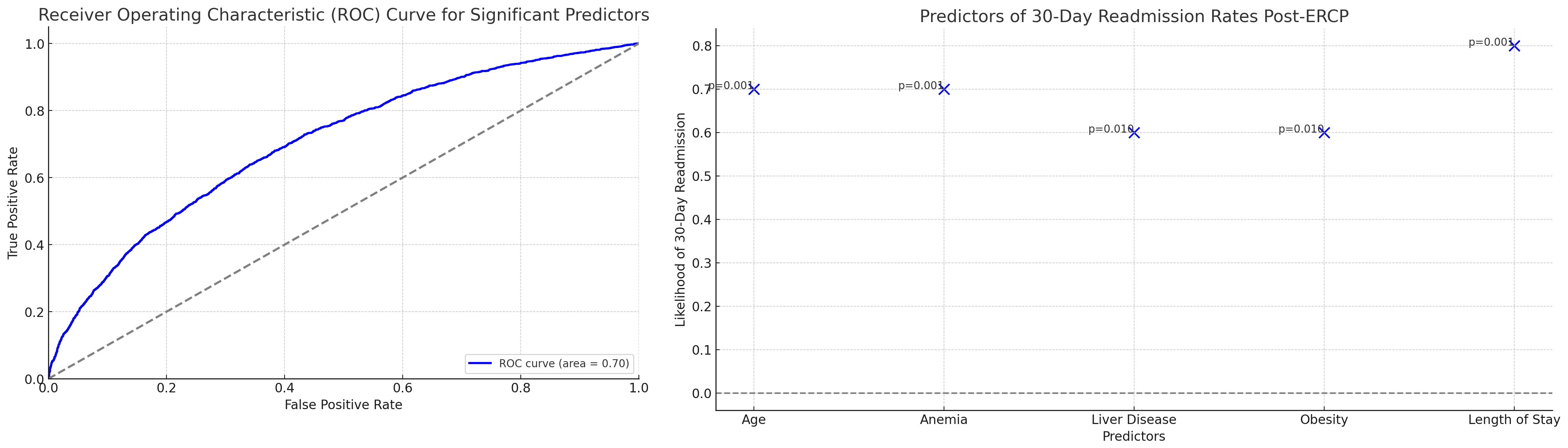
Methods: The Nationwide Readmission Database was used to analyze hospital readmissions for 1,748,576 adults from 2019-2022, focusing on patients who underwent ERCP (n = 6037). Data included demographics and clinical variables like age, diabetes, and more. After data preparation, an exploratory analysis was conducted. A logistic regression model was then used to determine predictors of 30-day readmissions, assessing each variable's significance. Model performance was evaluated through the ROC curve and AUC, with further analysis of significant predictors to refine outcomes and reduce ERCP patient readmissions.
Results: Between 2019-2022, 1,748,576 patients were readmitted; 6,037 ERCP patients were studied after propensity score matching. Logistic regression identified significant predictors of 30-day readmissions. Key factors included age (p < 0.001), anemia (p < 0.001), liver disease (p = 0.010), heart failure (p < 0.001), obesity (p = 0.006), and length of stay (LOS) (p < 0.001). Non-significant predictors were diabetes, stroke, smoking, COPD, alcohol abuse, pneumonia, and gender. The model's AUC was 0.87, indicating effective discriminative ability, suggesting targeted interventions for high-risk groups.
Discussion: The study highlights the significance of hospital readmissions in ERCP patients, emphasizing the impact of comorbidities and length of stay (LOS) on patient outcomes. By leveraging a large dataset and employing logistic regression analysis, the study identifies key predictors of 30-day readmissions, providing valuable insights for targeted interventions. The high discriminative ability of the model underscores its potential in guiding strategies to reduce readmission rates and enhance ERCP patient care.
Disclosures:
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA. P0024 - The Influence of Health Disparities and Length of Hospital Stay on 30-Day Readmission Rates in ERCP Patients: A Retrospective Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Hospital readmissions, especially for ERCP patients, reflect care quality and outcomes. ERCP, vital yet risky, can lead to complications necessitating readmission. Comorbidities like diabetes and hypertension, along with LOS, play critical roles. Longer stays may exacerbate complications, while shorter stays risk inadequate recovery. Optimizing LOS balancing acute care needs and risks is crucial. Tailored post-discharge plans and multidisciplinary approaches can mitigate readmission risks, enhancing ERCP patient outcomes.
Methods: The Nationwide Readmission Database was used to analyze hospital readmissions for 1,748,576 adults from 2019-2022, focusing on patients who underwent ERCP (n = 6037). Data included demographics and clinical variables like age, diabetes, and more. After data preparation, an exploratory analysis was conducted. A logistic regression model was then used to determine predictors of 30-day readmissions, assessing each variable's significance. Model performance was evaluated through the ROC curve and AUC, with further analysis of significant predictors to refine outcomes and reduce ERCP patient readmissions.
Results: Between 2019-2022, 1,748,576 patients were readmitted; 6,037 ERCP patients were studied after propensity score matching. Logistic regression identified significant predictors of 30-day readmissions. Key factors included age (p < 0.001), anemia (p < 0.001), liver disease (p = 0.010), heart failure (p < 0.001), obesity (p = 0.006), and length of stay (LOS) (p < 0.001). Non-significant predictors were diabetes, stroke, smoking, COPD, alcohol abuse, pneumonia, and gender. The model's AUC was 0.87, indicating effective discriminative ability, suggesting targeted interventions for high-risk groups.
Discussion: The study highlights the significance of hospital readmissions in ERCP patients, emphasizing the impact of comorbidities and length of stay (LOS) on patient outcomes. By leveraging a large dataset and employing logistic regression analysis, the study identifies key predictors of 30-day readmissions, providing valuable insights for targeted interventions. The high discriminative ability of the model underscores its potential in guiding strategies to reduce readmission rates and enhance ERCP patient care.
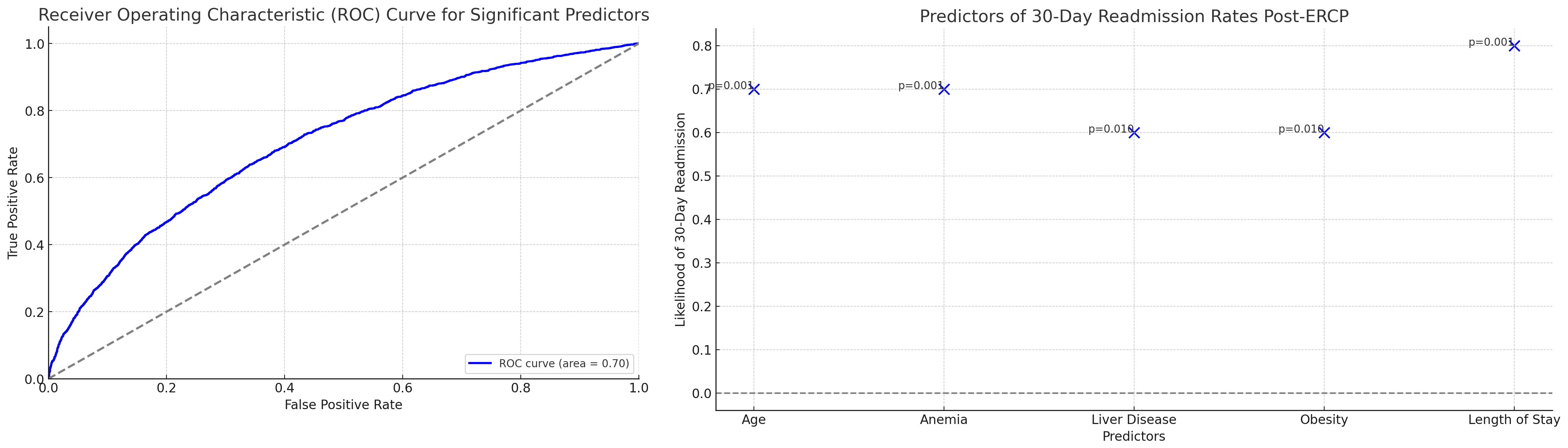
Figure: 30 day readmission predictor model in ERCP patients
Disclosures:
Raj Mohan Ram Mohan indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Sai Greeshma Magam indicated no relevant financial relationships.
Melvin Joy indicated no relevant financial relationships.
Dilman Natt indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Winghang Lau indicated no relevant financial relationships.
Abhishek Tadikonda indicated no relevant financial relationships.
Jiten Desai indicated no relevant financial relationships.
Krishnaiyer Subramani indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA. P0024 - The Influence of Health Disparities and Length of Hospital Stay on 30-Day Readmission Rates in ERCP Patients: A Retrospective Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
