Monday Poster Session
Category: Biliary/Pancreas
P1733 - EUS Findings in Patients With Isolated Pancreaticobiliary Ductal Dilatation on Abdominal Imaging With Normal LFTs
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Amber Hussain, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Amber Hussain, MD1, Abbinaya Elangovan, MD1, Andrew Catanzaro, MD2, Amitabh Chak, MD2, John Dumot, DO2, Gerard Isenberg, MD2, Brooke Glessing, MD2, Ashley Faulx, MD2
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Patients with isolated pancreaticobiliary (PB) duct dilation with normal liver function tests (LFTs) are often referred for endoscopic ultrasound (EUS). However, diagnostic yield of EUS is not well defined in this population.
Methods: Retrospective chart review was performed in a large tertiary PB referral center, from 2012-2023. Adults with bile duct (BD) dilation (CBD diameter ≥ 8 mm) on abdominal CT or MRI were included. Patients with abnormal LFTs, elevated CA 19-9, prior pancreatic duct (PD) or BD manipulation, prior PB surgery, or known PB malignancies were excluded. Imaging evidence of BD or PD stones, cysts, masses, strictures were excluded. EUS findings of duct caliber, presence of stones, parenchymal changes, or masses were collected. Charts were reviewed for PB pathology diagnosed after EUS was performed.
Results: 865 adults had EUS for the indication of PB duct dilation out of which 83 met criteria. There was an average of 5.5 years of follow-up. Baseline demographic features are listed in Table 1.
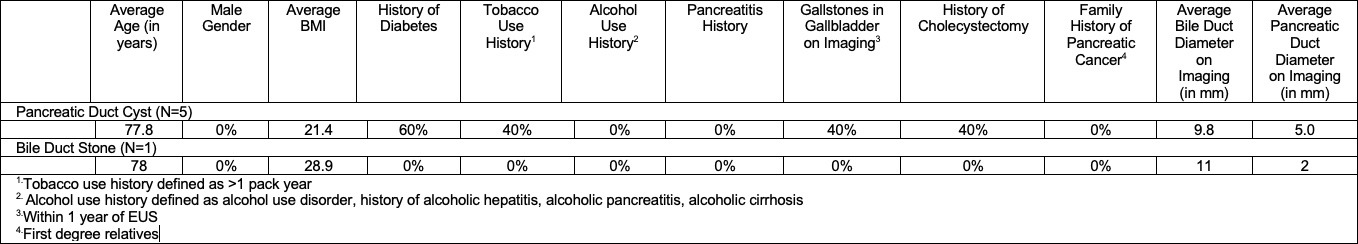
Among the 83 patients with biliary dilation on imaging, 30.1% also had PD dilation on imaging. 61.5% had demonstrable BD dilation on EUS, 22.9% had demonstrable PD dilation on EUS and 14.5% had both BD and PD duct dilation on EUS. 5 patients had a pancreatic cyst, the largest of which was 20mm in cross sectional diameter. 1 patient had a bile duct stone measuring 4mm in greatest dimension on EUS. EUS findings with associated risk factors can be seen in Image 1. These findings of pancreatic cysts and BD stone were not seen on initial imaging.
One patient who had a normal EUS with BD measuring 7.5mm was diagnosed with invasive gallbladder adenocarcinoma. This malignancy was diagnosed 1 year after initial EUS when the patient presented with cholecystitis and pathology from cholecystectomy revealed an occult adenocarcinoma. The BD remained normal on subsequent imaging during follow-up.
Discussion: Our 83 patients had normal abdominal imaging aside from PB duct dilation, however 6 patients had further abnormalities on EUS. No pancreatic or biliary malignancies were found on EUS in patients with normal LFTs and imaging. The finding of a negative EUS was a strong predictor of lack of pancreatic or bile duct pathology occurring in the near future. Our findings suggest that in the setting of isolated duct dilation, with otherwise normal imaging and LFTs, EUS may be warranted in some cases to investigate for occult pathology depending on clinical suspicion, symptoms, and quality of imaging.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Amber Hussain, MD1, Abbinaya Elangovan, MD1, Andrew Catanzaro, MD2, Amitabh Chak, MD2, John Dumot, DO2, Gerard Isenberg, MD2, Brooke Glessing, MD2, Ashley Faulx, MD2. P1733 - EUS Findings in Patients With Isolated Pancreaticobiliary Ductal Dilatation on Abdominal Imaging With Normal LFTs, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Patients with isolated pancreaticobiliary (PB) duct dilation with normal liver function tests (LFTs) are often referred for endoscopic ultrasound (EUS). However, diagnostic yield of EUS is not well defined in this population.
Methods: Retrospective chart review was performed in a large tertiary PB referral center, from 2012-2023. Adults with bile duct (BD) dilation (CBD diameter ≥ 8 mm) on abdominal CT or MRI were included. Patients with abnormal LFTs, elevated CA 19-9, prior pancreatic duct (PD) or BD manipulation, prior PB surgery, or known PB malignancies were excluded. Imaging evidence of BD or PD stones, cysts, masses, strictures were excluded. EUS findings of duct caliber, presence of stones, parenchymal changes, or masses were collected. Charts were reviewed for PB pathology diagnosed after EUS was performed.
Results: 865 adults had EUS for the indication of PB duct dilation out of which 83 met criteria. There was an average of 5.5 years of follow-up. Baseline demographic features are listed in Table 1.
Among the 83 patients with biliary dilation on imaging, 30.1% also had PD dilation on imaging. 61.5% had demonstrable BD dilation on EUS, 22.9% had demonstrable PD dilation on EUS and 14.5% had both BD and PD duct dilation on EUS. 5 patients had a pancreatic cyst, the largest of which was 20mm in cross sectional diameter. 1 patient had a bile duct stone measuring 4mm in greatest dimension on EUS. EUS findings with associated risk factors can be seen in Image 1. These findings of pancreatic cysts and BD stone were not seen on initial imaging.
One patient who had a normal EUS with BD measuring 7.5mm was diagnosed with invasive gallbladder adenocarcinoma. This malignancy was diagnosed 1 year after initial EUS when the patient presented with cholecystitis and pathology from cholecystectomy revealed an occult adenocarcinoma. The BD remained normal on subsequent imaging during follow-up.
Discussion: Our 83 patients had normal abdominal imaging aside from PB duct dilation, however 6 patients had further abnormalities on EUS. No pancreatic or biliary malignancies were found on EUS in patients with normal LFTs and imaging. The finding of a negative EUS was a strong predictor of lack of pancreatic or bile duct pathology occurring in the near future. Our findings suggest that in the setting of isolated duct dilation, with otherwise normal imaging and LFTs, EUS may be warranted in some cases to investigate for occult pathology depending on clinical suspicion, symptoms, and quality of imaging.
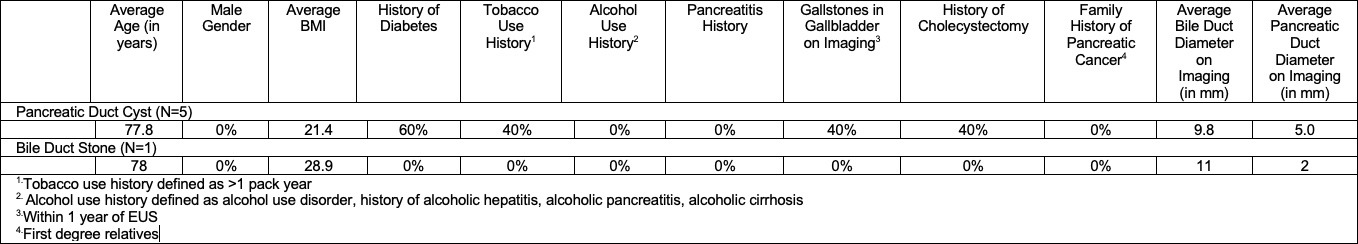
Figure: EUS Findings with Associated Risk Factors
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Amber Hussain indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Andrew Catanzaro indicated no relevant financial relationships.
Amitabh Chak: Lucid Diagnostics – Consultant, Grant/Research Support, Intellectual Property/Patents, Royalties, Stock Options, Stock-publicly held company(excluding mutual/index funds). MicroTech – Consultant. Steris – Consultant.
John Dumot indicated no relevant financial relationships.
Gerard Isenberg indicated no relevant financial relationships.
Brooke Glessing indicated no relevant financial relationships.
Ashley Faulx: Steris – Consultant.
Amber Hussain, MD1, Abbinaya Elangovan, MD1, Andrew Catanzaro, MD2, Amitabh Chak, MD2, John Dumot, DO2, Gerard Isenberg, MD2, Brooke Glessing, MD2, Ashley Faulx, MD2. P1733 - EUS Findings in Patients With Isolated Pancreaticobiliary Ductal Dilatation on Abdominal Imaging With Normal LFTs, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

