Monday Poster Session
Category: Biliary/Pancreas
P1752 - Cost-Effectiveness of Biodegradable Pancreatic Stents in Post-ERCP Pancreatitis Prophylaxis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Abdullah Abbasi, MBBS, MD, MRCP
Centre of Interventional Endoscopy at AdventHealth
Orlando, FL
Presenting Author(s)
Shyam Menon, MSc, MD, MBA1, Abdullah Abbasi, MBBS, MD, MRCP2
1The Royal Wolverhampton NHS Trust, Wolverhampton, England, United Kingdom; 2Centre of Interventional Endoscopy at AdventHealth, Orlando, FL
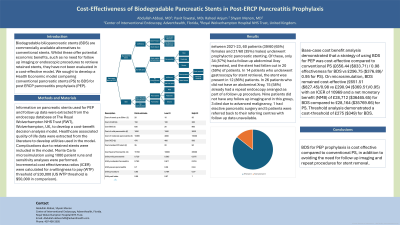
Introduction: Biodegradable biliopancreatic stents (BDS) are commercially available alternatives to conventional stents. Whilst these offer potential economic benefits, such as no need for follow up imaging or endoscopic procedures to retrieve retained stents, they have not been evaluated in a cost-effective model. We sought to develop a Health Economic model comparing conventional pancreatic stents (PS) to BDS for post ERCP pancreatitis prophylaxis (PEP).
Methods: Information on pancreatic stents used for PEP and follow up data were extracted from the endoscopy database at The Royal Wolverhampton NHS Trust (RWT), Wolverhampton, UK, to develop a cost-benefit decision analysis model. Healthcare associated quality of life data were extracted from the literature to develop utilities used in the model. Complications due to retained stents were included in the model. Monte Carlo microsimulation using 1000 patient runs and sensitivity analyses were performed. Incremental cost effectiveness ratios (ICER) were calculated for a willingness to pay (WTP) threshold of £30,000 (US WTP threshold is $50,000 in comparison).
Results: Between 2021-23, 60 patients (39/60 (65%) females and 21/60 (35%) males) underwent prophylactic pancreatic stenting. Of these, only 34 (57%) had a follow up abdominal Xray requested, and the stent had fallen out in 20 (59%) of patients. In 14 patients who underwent gastroscopy for stent retrieval, the stent was present in 12 (86%) patients. In 26 patients who did not have an abdominal Xray, 15 (58%) already had a repeat endoscopy arranged as part of a follow up procedure. Nine patients did not have any follow up imaging and in this group, 3 died due to advanced malignancy, 1 had elective pancreatic surgery and 5 patients were referred back to their referring centres with follow up data unavailable.
Base-case cost benefit analysis demonstrated that a strategy of using BDS for PEP was cost-effective compared to conventional PS (£656.44 ($833.71) / 0.98 effectiveness for BDS vs £296.75 ($376.89)/ 0.95 for PS). On microsimulation, BDS remained cost-effective (£651.51 ($827.45)/0.98 vs £290.94 ($369.51)/0.95) with an ICER of 10969 and a net monetary benefit (NMB) of £28,712 ($36465.65) for BDS compared to £28,164 ($35769.66) for PS. Threshold analysis demonstrated a cost-threshold of £275 ($349) for BDS.
Discussion:
BDS for PEP prophylaxis is cost effective compared to conventional PS, in addition to avoiding the need for follow up imaging and repeat procedures for stent removal.
Disclosures:
Shyam Menon, MSc, MD, MBA1, Abdullah Abbasi, MBBS, MD, MRCP2. P1752 - Cost-Effectiveness of Biodegradable Pancreatic Stents in Post-ERCP Pancreatitis Prophylaxis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Royal Wolverhampton NHS Trust, Wolverhampton, England, United Kingdom; 2Centre of Interventional Endoscopy at AdventHealth, Orlando, FL
Introduction: Biodegradable biliopancreatic stents (BDS) are commercially available alternatives to conventional stents. Whilst these offer potential economic benefits, such as no need for follow up imaging or endoscopic procedures to retrieve retained stents, they have not been evaluated in a cost-effective model. We sought to develop a Health Economic model comparing conventional pancreatic stents (PS) to BDS for post ERCP pancreatitis prophylaxis (PEP).
Methods: Information on pancreatic stents used for PEP and follow up data were extracted from the endoscopy database at The Royal Wolverhampton NHS Trust (RWT), Wolverhampton, UK, to develop a cost-benefit decision analysis model. Healthcare associated quality of life data were extracted from the literature to develop utilities used in the model. Complications due to retained stents were included in the model. Monte Carlo microsimulation using 1000 patient runs and sensitivity analyses were performed. Incremental cost effectiveness ratios (ICER) were calculated for a willingness to pay (WTP) threshold of £30,000 (US WTP threshold is $50,000 in comparison).
Results: Between 2021-23, 60 patients (39/60 (65%) females and 21/60 (35%) males) underwent prophylactic pancreatic stenting. Of these, only 34 (57%) had a follow up abdominal Xray requested, and the stent had fallen out in 20 (59%) of patients. In 14 patients who underwent gastroscopy for stent retrieval, the stent was present in 12 (86%) patients. In 26 patients who did not have an abdominal Xray, 15 (58%) already had a repeat endoscopy arranged as part of a follow up procedure. Nine patients did not have any follow up imaging and in this group, 3 died due to advanced malignancy, 1 had elective pancreatic surgery and 5 patients were referred back to their referring centres with follow up data unavailable.
Base-case cost benefit analysis demonstrated that a strategy of using BDS for PEP was cost-effective compared to conventional PS (£656.44 ($833.71) / 0.98 effectiveness for BDS vs £296.75 ($376.89)/ 0.95 for PS). On microsimulation, BDS remained cost-effective (£651.51 ($827.45)/0.98 vs £290.94 ($369.51)/0.95) with an ICER of 10969 and a net monetary benefit (NMB) of £28,712 ($36465.65) for BDS compared to £28,164 ($35769.66) for PS. Threshold analysis demonstrated a cost-threshold of £275 ($349) for BDS.
Discussion:
BDS for PEP prophylaxis is cost effective compared to conventional PS, in addition to avoiding the need for follow up imaging and repeat procedures for stent removal.
Disclosures:
Shyam Menon indicated no relevant financial relationships.
Abdullah Abbasi indicated no relevant financial relationships.
Shyam Menon, MSc, MD, MBA1, Abdullah Abbasi, MBBS, MD, MRCP2. P1752 - Cost-Effectiveness of Biodegradable Pancreatic Stents in Post-ERCP Pancreatitis Prophylaxis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
