Monday Poster Session
Category: Biliary/Pancreas
P1756 - Effect of Substance Use Counseling on Readmission Rates for Acute Alcohol-Associated Pancreatitis: A Prospective Cohort Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpeg.jpg)
Gurmehr Brar, MS, MD
University of Southern California
Culver City, CA
Presenting Author(s)
Award: Presidential Poster Award
Gurmehr Brar, MS, MD1, Matthew Chen, BA2, Dara Bruce, MSc3, Harry Trieu, MD4, Stephen Pandol, MD5, Christie Jeon, MS, Sc.D5, James Buxbaum, MD4
1University of Southern California, Culver City, CA; 2Keck School of Medicine of the University of Southern California, Torrance, CA; 3Keck School of Medicine of the University of Southern California, Glendale, CA; 4Keck School of Medicine of the University of Southern California, Los Angeles, CA; 5Cedars-Sinai Medical Center, Los Angeles, CA
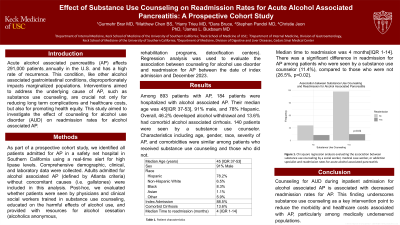
Introduction: Acute alcohol associated pancreatitis (AP) affects 291,000 patients annually in the U.S. and has a high rate of recurrence. This condition, like other alcohol associated gastrointestinal conditions, disproportionately impacts marginalized populations. Interventions aimed to address the underlying cause of AP, such as substance use counseling, are crucial not only for reducing long term complications and healthcare costs, but also for promoting health equity. This study aimed to investigate the effect of counseling for alcohol use disorder (AUD) on readmission rates for alcohol associated AP.
Methods: As part of a prospective cohort study, we identified all patients admitted for AP in a safety net hospital in Southern California using a real-time alert for high lipase levels. Comprehensive demographic, clinical, and laboratory data were collected. Adults admitted for alcohol associated AP (defined by Atlanta criteria) without concomitant causes (i.e. gallstones) were included in this analysis. Post-hoc, we evaluated whether patients were seen by substance use counselors, educated on the harmful effects of alcohol use, and provided with resources for alcohol cessation (alcoholics anonymous, rehabilitation programs, detoxification centers). Logistic regression analysis was used to evaluate the association between counseling for alcohol use disorder and readmission for AP between the date of index admission and December 2023.
Results: Among 893 patients with AP, 184 patients were hospitalized with alcohol associated AP. Their median age was 45[IQR 37-53], 91% were male, and 78% Hispanic. Overall, 46.2% developed alcohol withdrawal and 13.6% had comorbid alcohol associated cirrhosis. 140 patients were seen by a substance use counselor. Characteristics including age, gender, race, severity of AP, and comorbidities were similar among patients who received substance use counseling and those who did not. Median time to readmission was 4 months[IQR 1-14]. There was a significant difference in readmission for AP among patients who were seen by a substance use counselor (11.4%), compared to those who were not (26.5%, p=0.02).
Discussion: Counseling for AUD during inpatient admission for alcohol associated AP is associated with decreased readmission rates for AP. This finding underscores substance use counseling as a key intervention point to reduce the morbidity and healthcare costs associated with AP, particularly among medically underserved populations.
Disclosures:
Gurmehr Brar, MS, MD1, Matthew Chen, BA2, Dara Bruce, MSc3, Harry Trieu, MD4, Stephen Pandol, MD5, Christie Jeon, MS, Sc.D5, James Buxbaum, MD4. P1756 - Effect of Substance Use Counseling on Readmission Rates for Acute Alcohol-Associated Pancreatitis: A Prospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Gurmehr Brar, MS, MD1, Matthew Chen, BA2, Dara Bruce, MSc3, Harry Trieu, MD4, Stephen Pandol, MD5, Christie Jeon, MS, Sc.D5, James Buxbaum, MD4
1University of Southern California, Culver City, CA; 2Keck School of Medicine of the University of Southern California, Torrance, CA; 3Keck School of Medicine of the University of Southern California, Glendale, CA; 4Keck School of Medicine of the University of Southern California, Los Angeles, CA; 5Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Acute alcohol associated pancreatitis (AP) affects 291,000 patients annually in the U.S. and has a high rate of recurrence. This condition, like other alcohol associated gastrointestinal conditions, disproportionately impacts marginalized populations. Interventions aimed to address the underlying cause of AP, such as substance use counseling, are crucial not only for reducing long term complications and healthcare costs, but also for promoting health equity. This study aimed to investigate the effect of counseling for alcohol use disorder (AUD) on readmission rates for alcohol associated AP.
Methods: As part of a prospective cohort study, we identified all patients admitted for AP in a safety net hospital in Southern California using a real-time alert for high lipase levels. Comprehensive demographic, clinical, and laboratory data were collected. Adults admitted for alcohol associated AP (defined by Atlanta criteria) without concomitant causes (i.e. gallstones) were included in this analysis. Post-hoc, we evaluated whether patients were seen by substance use counselors, educated on the harmful effects of alcohol use, and provided with resources for alcohol cessation (alcoholics anonymous, rehabilitation programs, detoxification centers). Logistic regression analysis was used to evaluate the association between counseling for alcohol use disorder and readmission for AP between the date of index admission and December 2023.
Results: Among 893 patients with AP, 184 patients were hospitalized with alcohol associated AP. Their median age was 45[IQR 37-53], 91% were male, and 78% Hispanic. Overall, 46.2% developed alcohol withdrawal and 13.6% had comorbid alcohol associated cirrhosis. 140 patients were seen by a substance use counselor. Characteristics including age, gender, race, severity of AP, and comorbidities were similar among patients who received substance use counseling and those who did not. Median time to readmission was 4 months[IQR 1-14]. There was a significant difference in readmission for AP among patients who were seen by a substance use counselor (11.4%), compared to those who were not (26.5%, p=0.02).
Discussion: Counseling for AUD during inpatient admission for alcohol associated AP is associated with decreased readmission rates for AP. This finding underscores substance use counseling as a key intervention point to reduce the morbidity and healthcare costs associated with AP, particularly among medically underserved populations.
Disclosures:
Gurmehr Brar indicated no relevant financial relationships.
Matthew Chen indicated no relevant financial relationships.
Dara Bruce indicated no relevant financial relationships.
Harry Trieu indicated no relevant financial relationships.
Stephen Pandol indicated no relevant financial relationships.
Christie Jeon indicated no relevant financial relationships.
James Buxbaum indicated no relevant financial relationships.
Gurmehr Brar, MS, MD1, Matthew Chen, BA2, Dara Bruce, MSc3, Harry Trieu, MD4, Stephen Pandol, MD5, Christie Jeon, MS, Sc.D5, James Buxbaum, MD4. P1756 - Effect of Substance Use Counseling on Readmission Rates for Acute Alcohol-Associated Pancreatitis: A Prospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

