Monday Poster Session
Category: Biliary/Pancreas
P1764 - Compliance to NCCN Tumor Gene Profiling Guidelines in Pancreatic Ductal Adenocarcinoma: A Large Multi-Center Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Malak Al-Bitar, MD
Geisinger Health System
Danville, PA
Presenting Author(s)
Award: Presidential Poster Award
Malak Al-Bitar, MD1, Konstantinos Damiris, DO2, Vyshnavi Kodali, DO2, Idorenyin Udoeyo, MPH1, Bradley D.. Confer, DO1
1Geisinger Health System, Danville, PA; 2Geisinger Medical Center, Danville, PA
Introduction: Pancreatic ductal adenocarcinoma (PDAC) is frequently diagnosed in later stages, contributing to its high mortality. PDAC is associated with genetic mutations such as KRAS, found in ~85% of cases. In 2019, the National Comprehensive Cancer Network (NCCN) recommended genetic testing, including universal germline testing and tumor gene profiling along with microsatellite instability (MSI)/mismatch repair (MMR) testing (Next-Generation Sequencing: NGS) in all PDAC cases. We aim to evaluate compliance with NGS in a large tertiary rural health system and determine factors influencing testing acquisition.
Methods: We performed a retrospective, observational study of patients with biopsy-proven PDAC within an academic health system between 2018 and June 2023. We recorded NGS referrals and results. Demographics, treatments, and outcomes were also documented. Chi-square and Wilcoxon two-sample tests were conducted for categorical and continuous characteristics, respectively. A Cochran-Armitage test was conducted to examine the NGS offering over the years. A multivariable logistic regression analysis was performed to determine factors associated with NGS testing. A p < 0.05 was considered significant.
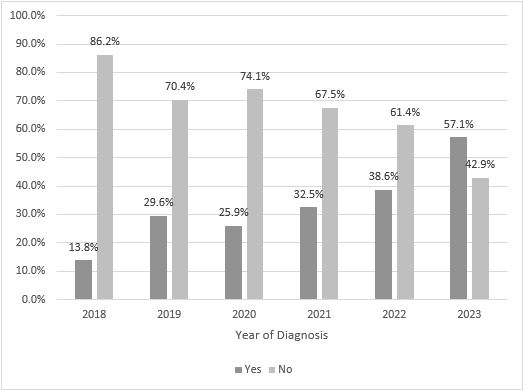
Results: 587 patients with PDAC were included. The median age at diagnosis was 70 years; 50.4% were males, and 97.4% Caucasian. 182 (31.1%) patients underwent NGS. Figure 1 demonstrates the frequency of patients offered NGS per year. There is a significant trend of NGS being offered over time, with more patients undergoing testing following the 2019 NCCN recommendations (p< 0.0001). Characteristics of patients undergoing NGS are outlined in Table 1. In multivariable analysis, NGS was offered more frequently over the years, to younger patients, those with lower ECOG scores and those who underwent palliative chemotherapy. Microsatellite instability was encountered in 4 (2.3%) of patients. The most common mutation detected was K-RAS in 157 (90.8%) patients, of which G12D was seen in 38.9% and G12V in 29.3%. Additionally, P53 was aberrant in 68.8%, CDKN2A/B in 41.2%, SMAD4 in 34.1%, BRCA 2 in 15.9%, and ATM in 6.4%.
Discussion: Though there has been an overall improvement regarding NGS testing in patients with PDAC since the 2019 NCCN recommendation, this study highlights that universal testing remains inconsistent. Early genetic testing results may influence treatment and patient outcomes. Efforts should focus on implementing feasible testing more systematically.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Malak Al-Bitar, MD1, Konstantinos Damiris, DO2, Vyshnavi Kodali, DO2, Idorenyin Udoeyo, MPH1, Bradley D.. Confer, DO1. P1764 - Compliance to NCCN Tumor Gene Profiling Guidelines in Pancreatic Ductal Adenocarcinoma: A Large Multi-Center Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Malak Al-Bitar, MD1, Konstantinos Damiris, DO2, Vyshnavi Kodali, DO2, Idorenyin Udoeyo, MPH1, Bradley D.. Confer, DO1
1Geisinger Health System, Danville, PA; 2Geisinger Medical Center, Danville, PA
Introduction: Pancreatic ductal adenocarcinoma (PDAC) is frequently diagnosed in later stages, contributing to its high mortality. PDAC is associated with genetic mutations such as KRAS, found in ~85% of cases. In 2019, the National Comprehensive Cancer Network (NCCN) recommended genetic testing, including universal germline testing and tumor gene profiling along with microsatellite instability (MSI)/mismatch repair (MMR) testing (Next-Generation Sequencing: NGS) in all PDAC cases. We aim to evaluate compliance with NGS in a large tertiary rural health system and determine factors influencing testing acquisition.
Methods: We performed a retrospective, observational study of patients with biopsy-proven PDAC within an academic health system between 2018 and June 2023. We recorded NGS referrals and results. Demographics, treatments, and outcomes were also documented. Chi-square and Wilcoxon two-sample tests were conducted for categorical and continuous characteristics, respectively. A Cochran-Armitage test was conducted to examine the NGS offering over the years. A multivariable logistic regression analysis was performed to determine factors associated with NGS testing. A p < 0.05 was considered significant.
Results: 587 patients with PDAC were included. The median age at diagnosis was 70 years; 50.4% were males, and 97.4% Caucasian. 182 (31.1%) patients underwent NGS. Figure 1 demonstrates the frequency of patients offered NGS per year. There is a significant trend of NGS being offered over time, with more patients undergoing testing following the 2019 NCCN recommendations (p< 0.0001). Characteristics of patients undergoing NGS are outlined in Table 1. In multivariable analysis, NGS was offered more frequently over the years, to younger patients, those with lower ECOG scores and those who underwent palliative chemotherapy. Microsatellite instability was encountered in 4 (2.3%) of patients. The most common mutation detected was K-RAS in 157 (90.8%) patients, of which G12D was seen in 38.9% and G12V in 29.3%. Additionally, P53 was aberrant in 68.8%, CDKN2A/B in 41.2%, SMAD4 in 34.1%, BRCA 2 in 15.9%, and ATM in 6.4%.
Discussion: Though there has been an overall improvement regarding NGS testing in patients with PDAC since the 2019 NCCN recommendation, this study highlights that universal testing remains inconsistent. Early genetic testing results may influence treatment and patient outcomes. Efforts should focus on implementing feasible testing more systematically.
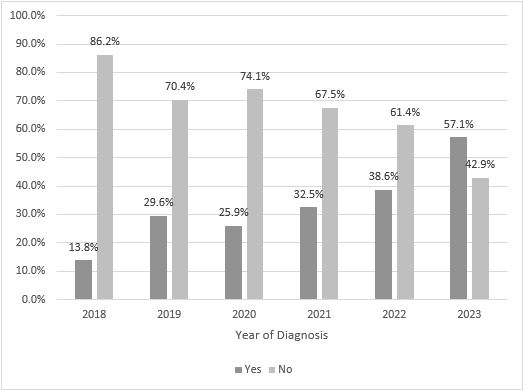
Figure: Figure 1. Offering of next-generation sequencing per number of cases each year (Cochran-Armitage test, p<0.0001)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Malak Al-Bitar indicated no relevant financial relationships.
Konstantinos Damiris indicated no relevant financial relationships.
Vyshnavi Kodali indicated no relevant financial relationships.
Idorenyin Udoeyo indicated no relevant financial relationships.
Bradley Confer: Boston Scientific Corporation – Consultant. Exact Sciences – Advisory Committee/Board Member, FDA advisory panel.
Malak Al-Bitar, MD1, Konstantinos Damiris, DO2, Vyshnavi Kodali, DO2, Idorenyin Udoeyo, MPH1, Bradley D.. Confer, DO1. P1764 - Compliance to NCCN Tumor Gene Profiling Guidelines in Pancreatic Ductal Adenocarcinoma: A Large Multi-Center Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

