Monday Poster Session
Category: Biliary/Pancreas
P1765 - Demographic Inequalities in Participant Enrollment in Clinical Trials for Acute And Chronic Pancreatitis in the United States
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Wissam Ghusn, MD
Boston Medical Center
Boston, MA
Presenting Author(s)
Wissam Ghusn, MD1, Hector F.. Reyes Santiago, 2, Khushboo Gala, MBBS3, Serena Rahme, MD4, Marita Salame, MD4, Rudy Mrad, MD4, Jeremy Chimene-weiss, MD1, Victor Chedid, MD, MS4
1Boston Medical Center, Boston, MA; 2University of Puerto Rico School of Medicine, Guaynabo, Puerto Rico; 3Mayo Clinic School of Graduate Medical Education, Rochester, MN; 4Mayo Clinic, Rochester, MN
Introduction: Pancreatitis is one of the most common causes of gastrointestinal disease hospitalizations in the United States (US). The medical burden of pancreatitis extends beyond its immediate symptoms, impacting patients' quality of life and necessitating extensive healthcare resources. Several randomized clinical trials (RCTs) have been undertaken to investigate therapeutic approaches for pancreatitis. Notably, the pharmacokinetics and pharmacodynamics of medications utilized have been shown to be significantly influenced by factors such as sex, age, and race. Our objective is to evaluate whether there are any disparities in age, sex, race, or ethnicity within the conducted RCTs for pancreatitis.
Methods: We conducted an extensive search for all clinical trials involving patients with pancreatitis, registered on clinicaltrials.gov in the US until June 2023. We implemented various filters to encompass all completed interventional trials in phases 2, 3, and 4, without limitations on the trial initiation or completion dates. Mean age, age categories, percentage of female participants, racial and ethnic distribution of trial participants were collected for each of acute and chronic pancreatitis separately.
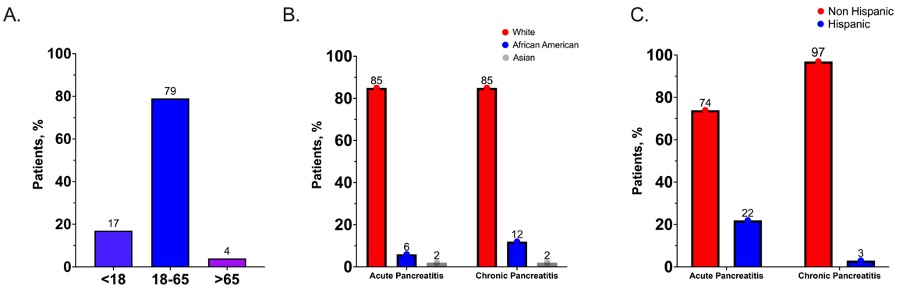
Results: We incorporated a total of 39 distinct trials, involving 2452 patients diagnosed with pancreatitis (11 with acute pancreatitis and 28 with chronic pancreatitis). Comprehensive demographic data is presented in Table 1. Notably, only 4% of patients with chronic pancreatitis were older than 65 years (Figure 1A). In the case of acute and chronic pancreatitis, 56% and 45% of the patients were female, respectively. The majority of participants were of White ethnicity (85% and 96%) in acute and chronic pancreatitis, with a remarkable smaller percentage of African American individuals (6% and 12%), and Asian individuals (2% for both) (Figure 1B). Concerning ethnicity, the overwhelming majority were non-Hispanic compared to Hispanic, accounting for 74% vs. 24% in acute pancreatitis and 97% vs. 3% in chronic pancreatitis (Figure 1C).
Discussion: In this study, we highlight significant age, racial, and ethnic imbalances in participant recruitment for clinical trials related to acute and chronic pancreatitis in the US. It is imperative to employ more efficient recruitment strategies to ensure the inclusion of diverse and representative populations, potentially preventing disparities in future care and guidelines for pancreatitis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Wissam Ghusn, MD1, Hector F.. Reyes Santiago, 2, Khushboo Gala, MBBS3, Serena Rahme, MD4, Marita Salame, MD4, Rudy Mrad, MD4, Jeremy Chimene-weiss, MD1, Victor Chedid, MD, MS4. P1765 - Demographic Inequalities in Participant Enrollment in Clinical Trials for Acute And Chronic Pancreatitis in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Boston Medical Center, Boston, MA; 2University of Puerto Rico School of Medicine, Guaynabo, Puerto Rico; 3Mayo Clinic School of Graduate Medical Education, Rochester, MN; 4Mayo Clinic, Rochester, MN
Introduction: Pancreatitis is one of the most common causes of gastrointestinal disease hospitalizations in the United States (US). The medical burden of pancreatitis extends beyond its immediate symptoms, impacting patients' quality of life and necessitating extensive healthcare resources. Several randomized clinical trials (RCTs) have been undertaken to investigate therapeutic approaches for pancreatitis. Notably, the pharmacokinetics and pharmacodynamics of medications utilized have been shown to be significantly influenced by factors such as sex, age, and race. Our objective is to evaluate whether there are any disparities in age, sex, race, or ethnicity within the conducted RCTs for pancreatitis.
Methods: We conducted an extensive search for all clinical trials involving patients with pancreatitis, registered on clinicaltrials.gov in the US until June 2023. We implemented various filters to encompass all completed interventional trials in phases 2, 3, and 4, without limitations on the trial initiation or completion dates. Mean age, age categories, percentage of female participants, racial and ethnic distribution of trial participants were collected for each of acute and chronic pancreatitis separately.
Results: We incorporated a total of 39 distinct trials, involving 2452 patients diagnosed with pancreatitis (11 with acute pancreatitis and 28 with chronic pancreatitis). Comprehensive demographic data is presented in Table 1. Notably, only 4% of patients with chronic pancreatitis were older than 65 years (Figure 1A). In the case of acute and chronic pancreatitis, 56% and 45% of the patients were female, respectively. The majority of participants were of White ethnicity (85% and 96%) in acute and chronic pancreatitis, with a remarkable smaller percentage of African American individuals (6% and 12%), and Asian individuals (2% for both) (Figure 1B). Concerning ethnicity, the overwhelming majority were non-Hispanic compared to Hispanic, accounting for 74% vs. 24% in acute pancreatitis and 97% vs. 3% in chronic pancreatitis (Figure 1C).
Discussion: In this study, we highlight significant age, racial, and ethnic imbalances in participant recruitment for clinical trials related to acute and chronic pancreatitis in the US. It is imperative to employ more efficient recruitment strategies to ensure the inclusion of diverse and representative populations, potentially preventing disparities in future care and guidelines for pancreatitis.
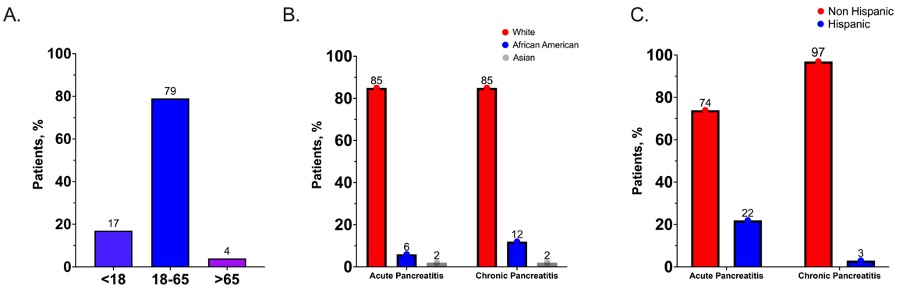
Figure: Figure 1: Age (A), race (B), and ethnic (C) distribution of enrolled participants in US clinical trials for acute and chronic pancreatitis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Wissam Ghusn indicated no relevant financial relationships.
Hector Reyes Santiago indicated no relevant financial relationships.
Khushboo Gala indicated no relevant financial relationships.
Serena Rahme indicated no relevant financial relationships.
Marita Salame indicated no relevant financial relationships.
Rudy Mrad indicated no relevant financial relationships.
Jeremy Chimene-weiss indicated no relevant financial relationships.
Victor Chedid indicated no relevant financial relationships.
Wissam Ghusn, MD1, Hector F.. Reyes Santiago, 2, Khushboo Gala, MBBS3, Serena Rahme, MD4, Marita Salame, MD4, Rudy Mrad, MD4, Jeremy Chimene-weiss, MD1, Victor Chedid, MD, MS4. P1765 - Demographic Inequalities in Participant Enrollment in Clinical Trials for Acute And Chronic Pancreatitis in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
