Monday Poster Session
Category: Biliary/Pancreas
P1815 - Biloma Presenting as Refractory Right Upper Quadrant Abdominal Pain Post Cholecystectomy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Yannis Lafazanos, DO
Advocate Lutheran General
Park Ridge, IL
Presenting Author(s)
Yannis Lafazanos, DO1, Abdulkareem Abuzir, DO1, Nicolas Prabhakar, DO1, Robert Zimmanck, MD1, Eli D. Ehrenpreis, MD, FACG2
1Advocate Lutheran General, Park Ridge, IL; 2E2Bio Consultants, Evanston, IL
Introduction: Anomalous biliary ducts may be strikingly common, given the high degree of variation during the primitive foregut’s development, but are normally inconsequential. Variation, however, causes complications in the setting of surgery, specifically in cholecystectomies. Our patient suffered post-surgical complications, including infection and chronic pain, from a damaged anomalous bile duct. Damage to anomalous bile ducts cause complications to the postoperative course of about 13% of cholecystectomies. We hope that this report highlights a relatively common, but under-appreciated complication of an exceedingly common surgery.
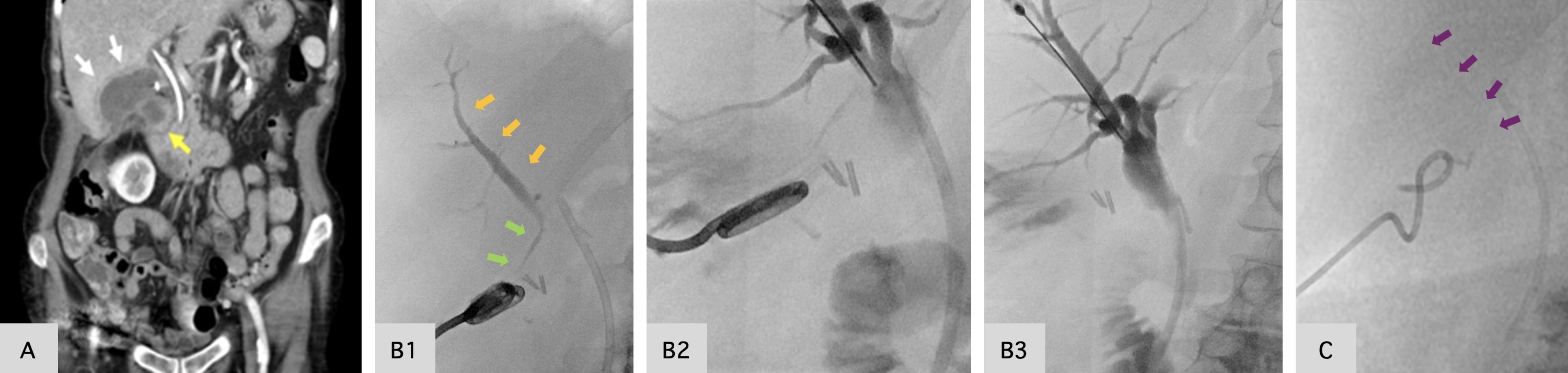
Case Description/Methods: A 70-year-old female with a history of cholecystitis, now 2-months status post cholecystectomy, presented to the ED with refractory right upper quadrant (RUQ) abdominal pain. Her postoperative evaluation had already included a HIDA scan, on postoperative day (POD) #6, suspicious for biliary leak and ERCP with common bile duct (CBD) stent placement for preferential draining on POD#7.CT scan now showed interval development of a loculated fluid collection in the gallbladder fossa (Image 1, A). Intravenous antibiotics were initiated, and a percutaneous cholecystostomy tube (PCT) was placed. Six days later, POD#67, a sinogram showed slow retrograde opacification of an isolated right posterior sectoral duct injury (RPSD), which was anomalously connected to the absent gallbladder and actively feeding the open fossa, causing the biloma (Image 1, B1). Subsequent percutaneous cholangiogram confirmed the RPSD’s connection to the biliary system, but noted minimal opacification with contrast, meaning it was too small for direct catheterization or embolization (Image 1, B2-3). Her RUQ pain improved with the PCT, and she was stabilized for discharge. Two weeks later, on POD#86, repeat sinography demonstrated obliteration of the patent duct, and the cholecystostomy tube was removed (Image 1, C). Her CBD stent was removed via repeat ERCP on POD#96.
Discussion: Anomalies of the biliary system typically have no clinical significance but given fewer than half of healthy individuals have “normal” anatomy, complications are likely to occur. In many, rupture of anomalous ducts may cause no or mild pain, ultimately with self-resolution without intervention. In our patient, multiple scans, stents, and tubes were needed. Stressing the surgical cholangiogram and heightening our clinical suspicion for bile duct injury may have prevented or limited complications.
Disclosures:
Yannis Lafazanos, DO1, Abdulkareem Abuzir, DO1, Nicolas Prabhakar, DO1, Robert Zimmanck, MD1, Eli D. Ehrenpreis, MD, FACG2. P1815 - Biloma Presenting as Refractory Right Upper Quadrant Abdominal Pain Post Cholecystectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Advocate Lutheran General, Park Ridge, IL; 2E2Bio Consultants, Evanston, IL
Introduction: Anomalous biliary ducts may be strikingly common, given the high degree of variation during the primitive foregut’s development, but are normally inconsequential. Variation, however, causes complications in the setting of surgery, specifically in cholecystectomies. Our patient suffered post-surgical complications, including infection and chronic pain, from a damaged anomalous bile duct. Damage to anomalous bile ducts cause complications to the postoperative course of about 13% of cholecystectomies. We hope that this report highlights a relatively common, but under-appreciated complication of an exceedingly common surgery.
Case Description/Methods: A 70-year-old female with a history of cholecystitis, now 2-months status post cholecystectomy, presented to the ED with refractory right upper quadrant (RUQ) abdominal pain. Her postoperative evaluation had already included a HIDA scan, on postoperative day (POD) #6, suspicious for biliary leak and ERCP with common bile duct (CBD) stent placement for preferential draining on POD#7.CT scan now showed interval development of a loculated fluid collection in the gallbladder fossa (Image 1, A). Intravenous antibiotics were initiated, and a percutaneous cholecystostomy tube (PCT) was placed. Six days later, POD#67, a sinogram showed slow retrograde opacification of an isolated right posterior sectoral duct injury (RPSD), which was anomalously connected to the absent gallbladder and actively feeding the open fossa, causing the biloma (Image 1, B1). Subsequent percutaneous cholangiogram confirmed the RPSD’s connection to the biliary system, but noted minimal opacification with contrast, meaning it was too small for direct catheterization or embolization (Image 1, B2-3). Her RUQ pain improved with the PCT, and she was stabilized for discharge. Two weeks later, on POD#86, repeat sinography demonstrated obliteration of the patent duct, and the cholecystostomy tube was removed (Image 1, C). Her CBD stent was removed via repeat ERCP on POD#96.
Discussion: Anomalies of the biliary system typically have no clinical significance but given fewer than half of healthy individuals have “normal” anatomy, complications are likely to occur. In many, rupture of anomalous ducts may cause no or mild pain, ultimately with self-resolution without intervention. In our patient, multiple scans, stents, and tubes were needed. Stressing the surgical cholangiogram and heightening our clinical suspicion for bile duct injury may have prevented or limited complications.
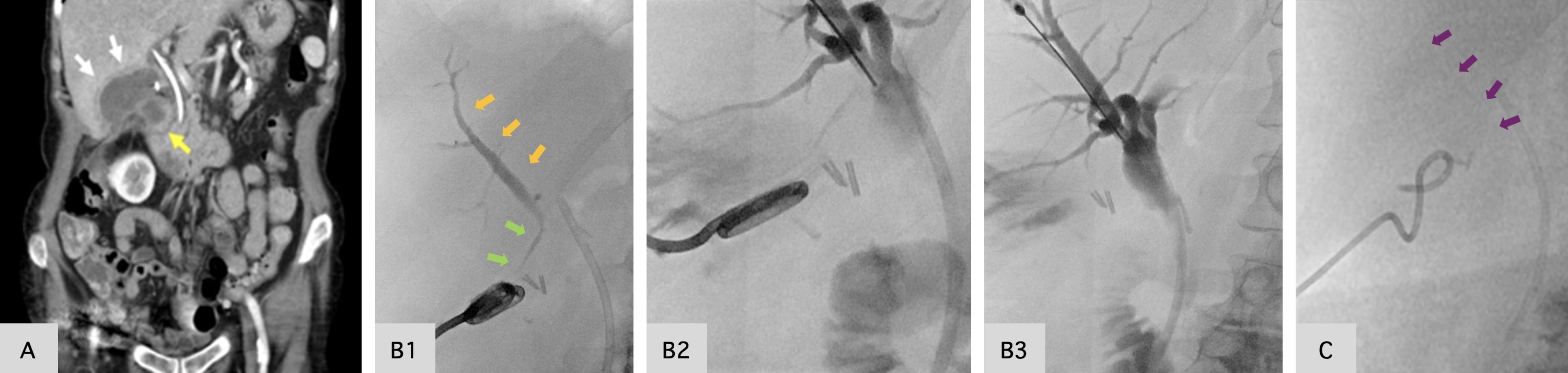
Figure: Image 1. Serial abdominal imaging with CT and sinography. (A) indicates a surgically absent gallbladder, and a thick-walled, loculated fluid collection in the gallbladder fossa, with a horizontal component (white arrows) measuring 5.9 x 3.0 cm (about 1.18 in). (B1) indicates right posterior sectoral duct injury (green arrows) with the uptake of contrast via the open bile duct and into the biliary system, indicated as slow opacification after contrast injection (orange arrows). (B2-3) shows uptake of contrast media and opacification of the biliary system, sequentially, from the initial right posterior sectoral duct defect, meeting at the common bile duct. (C) repeat sinogram, noting no uptake of contrast media (purple arrows), no residual cavity or fistula, with resolution of bile leak.
Disclosures:
Yannis Lafazanos indicated no relevant financial relationships.
Abdulkareem Abuzir indicated no relevant financial relationships.
Nicolas Prabhakar indicated no relevant financial relationships.
Robert Zimmanck indicated no relevant financial relationships.
Eli Ehrenpreis: E2Bio Life Sciences – Intellectual Property/Patents, Owner/Ownership Interest, Stock-privately held company.
Yannis Lafazanos, DO1, Abdulkareem Abuzir, DO1, Nicolas Prabhakar, DO1, Robert Zimmanck, MD1, Eli D. Ehrenpreis, MD, FACG2. P1815 - Biloma Presenting as Refractory Right Upper Quadrant Abdominal Pain Post Cholecystectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
