Monday Poster Session
Category: Biliary/Pancreas
P1831 - Necrotizing Pancreatitis With Gastric and Colonic Fistulae
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- GG
Gaurav Gopu
Medical College of Georgia at Augusta University
Cumming, GA
Presenting Author(s)
Gaurav Gopu, 1, Amit Hudgi, MD2, Abdul-Rahman Abualruz, MD3, Ahmad Alkaddour, MD2, John Erikson Yap, MD, MBA, FACG4, Viveksandeep Thoguluva Chandrasekar, MBBS2
1Medical College of Georgia at Augusta University, Cumming, GA; 2Medical College of Georgia at Augusta University, Augusta, GA; 3Medical College of Georgia, Augusta University, Augusta, GA; 4Metrodora Institute, West Valley City, UT
Introduction: Gastrointestinal fistulas are rare but potentially fatal complications of necrotizing pancreatitis. Despite being well-documented, the management remains complex. We present an interesting case of necrotizing pancreatitis complicated by gastrointestinal fistulae to the stomach and colon, due to underlying pancreatic cancer.
Case Description/Methods: A 48-year-old male with history of recurrent pancreatitis with necrosis at outside facility presented with acute onset of severe epigastric abdominal pain accompanied by weakness, chills and reduced oral intake due to pain. On examination, he was found to be altered, with a heart rate of 115 beats/min and blood pressure of 100/70 mmHg. Prior imaging studies had not shown any pancreatic mass and he had undergone endoscopic ultrasound guided aspiration of a 4.5 cm peri-pancreatic fluid collection for persistent pain, 6 weeks prior, did not show any malignant cells on cytology.
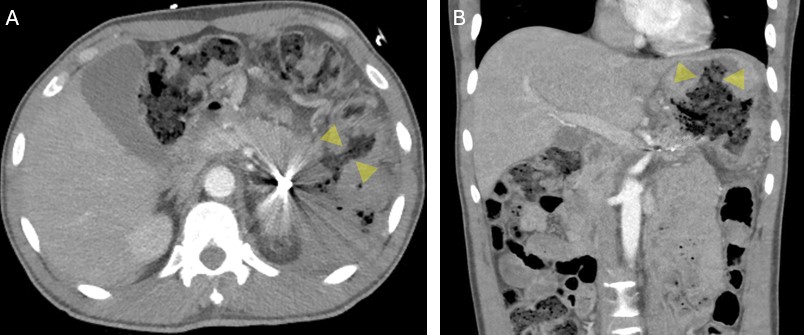
Laboratory findings showed hemoglobin level of 10 g/dL and WBC count of 21,000 cells/mm³. CA 19-9 was elevated at 871.2. CT scan of the abdomen and pelvis revealed progressive necrotizing pancreatitis with substantial defects in the walls of the stomach and colon, resulting in fistulous connections to a large walled-off necrosis in the left upper quadrant (Figure A and B).
The patient was initially conservatively managed with antibiotics, pain control, and parenteral nutrition. A multidisciplinary approach was employed to address symptomatic relief, infection control, and strategic planning for potential interventions given the complex and evolving nature of his condition. Despite initial management, his symptoms continued to deteriorate, leading to the decision for surgical necrosectomy. On exploratory laparotomy, he was found to have pancreatic cancer invading the gastric and colonic walls and the spleen and he underwent distal pancreatectomy with splenectomy, hemicolectomy and partial gastrectomy with pathology showing invasive pancreatic adenocarcinoma. He is currently considering hospice given his poor prognosis and persistent pain.
Discussion: The emergence of gastrointestinal fistulas following necrotizing pancreatitis poses substantial management complexities. Early identification of pancreatic cancer can also be critical and challenging, requiring a comprehensive and multidisciplinary approach. Current literature underscores the scarcity of comprehensive guidelines, highlighting the need for further research to refine therapeutic strategies and optimize patient outcomes.
Disclosures:
Gaurav Gopu, 1, Amit Hudgi, MD2, Abdul-Rahman Abualruz, MD3, Ahmad Alkaddour, MD2, John Erikson Yap, MD, MBA, FACG4, Viveksandeep Thoguluva Chandrasekar, MBBS2. P1831 - Necrotizing Pancreatitis With Gastric and Colonic Fistulae, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Medical College of Georgia at Augusta University, Cumming, GA; 2Medical College of Georgia at Augusta University, Augusta, GA; 3Medical College of Georgia, Augusta University, Augusta, GA; 4Metrodora Institute, West Valley City, UT
Introduction: Gastrointestinal fistulas are rare but potentially fatal complications of necrotizing pancreatitis. Despite being well-documented, the management remains complex. We present an interesting case of necrotizing pancreatitis complicated by gastrointestinal fistulae to the stomach and colon, due to underlying pancreatic cancer.
Case Description/Methods: A 48-year-old male with history of recurrent pancreatitis with necrosis at outside facility presented with acute onset of severe epigastric abdominal pain accompanied by weakness, chills and reduced oral intake due to pain. On examination, he was found to be altered, with a heart rate of 115 beats/min and blood pressure of 100/70 mmHg. Prior imaging studies had not shown any pancreatic mass and he had undergone endoscopic ultrasound guided aspiration of a 4.5 cm peri-pancreatic fluid collection for persistent pain, 6 weeks prior, did not show any malignant cells on cytology.
Laboratory findings showed hemoglobin level of 10 g/dL and WBC count of 21,000 cells/mm³. CA 19-9 was elevated at 871.2. CT scan of the abdomen and pelvis revealed progressive necrotizing pancreatitis with substantial defects in the walls of the stomach and colon, resulting in fistulous connections to a large walled-off necrosis in the left upper quadrant (Figure A and B).
The patient was initially conservatively managed with antibiotics, pain control, and parenteral nutrition. A multidisciplinary approach was employed to address symptomatic relief, infection control, and strategic planning for potential interventions given the complex and evolving nature of his condition. Despite initial management, his symptoms continued to deteriorate, leading to the decision for surgical necrosectomy. On exploratory laparotomy, he was found to have pancreatic cancer invading the gastric and colonic walls and the spleen and he underwent distal pancreatectomy with splenectomy, hemicolectomy and partial gastrectomy with pathology showing invasive pancreatic adenocarcinoma. He is currently considering hospice given his poor prognosis and persistent pain.
Discussion: The emergence of gastrointestinal fistulas following necrotizing pancreatitis poses substantial management complexities. Early identification of pancreatic cancer can also be critical and challenging, requiring a comprehensive and multidisciplinary approach. Current literature underscores the scarcity of comprehensive guidelines, highlighting the need for further research to refine therapeutic strategies and optimize patient outcomes.
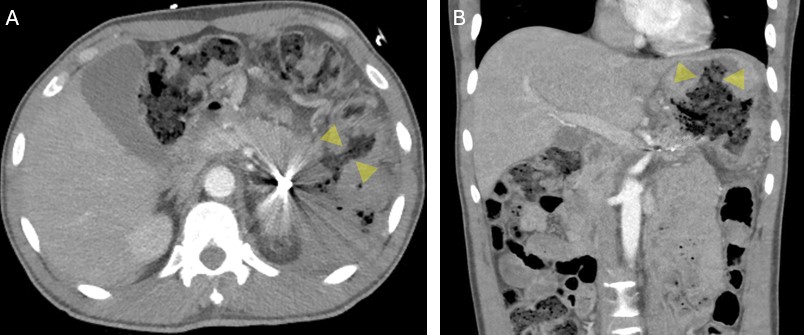
Figure: Figure 1: Axial (A) and Coronal (B) CT images of the abdomen with IV contrast demonstrate pancreatic necrotic collection fistulous communication with the splenic flexure of the colon (arrowheads, A), and the stomach (arrowheads, B).
Disclosures:
Gaurav Gopu indicated no relevant financial relationships.
Amit Hudgi indicated no relevant financial relationships.
Abdul-Rahman Abualruz indicated no relevant financial relationships.
Ahmad Alkaddour indicated no relevant financial relationships.
John Erikson Yap indicated no relevant financial relationships.
Viveksandeep Thoguluva Chandrasekar indicated no relevant financial relationships.
Gaurav Gopu, 1, Amit Hudgi, MD2, Abdul-Rahman Abualruz, MD3, Ahmad Alkaddour, MD2, John Erikson Yap, MD, MBA, FACG4, Viveksandeep Thoguluva Chandrasekar, MBBS2. P1831 - Necrotizing Pancreatitis With Gastric and Colonic Fistulae, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
