Monday Poster Session
Category: Biliary/Pancreas
P1840 - Diabetic Ketoacidosis as Early Presentation of Pancreatic Adenocarcinoma
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MB
Marlon J. Brewer, MD
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Marlon J. Brewer, MD, Edward Cytryn, MD, Valerie Moscoso, MD, Eric Barna, MD, Aimee L. Lucas, MD, MS
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Pancreatic Ductal Adenocarcinoma (PDAC) is the 3rd leading cause of cancer related death in the United States. The bidirectional relationship between PDAC and diabetes is under study to determine if changes in metabolic parameters can predict cancer development. While new-onset diabetes is a well-described early manifestation of PDAC, we report a rare case of diabetic ketoacidosis (DKA) as the early presentation of PDAC.
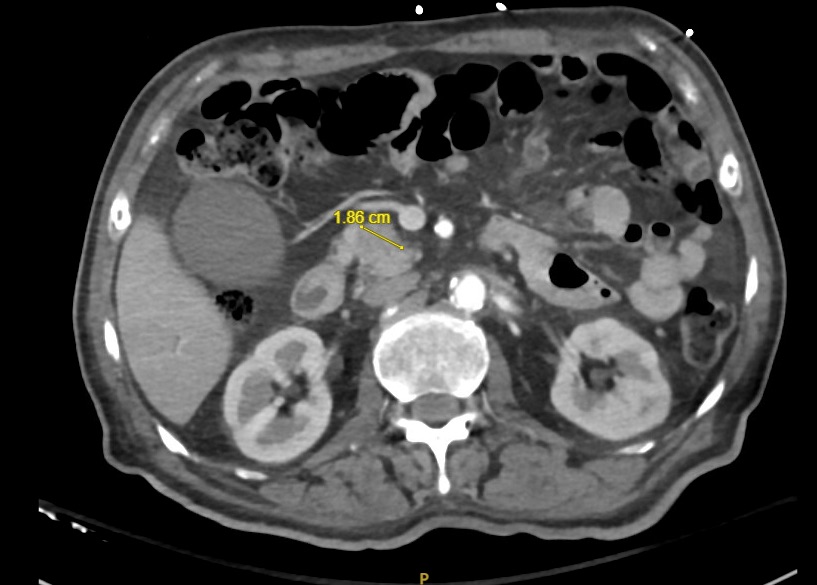
Case Description/Methods: A 68-year-old man with chronic non-insulin dependent type 2 diabetes (T2DM) presented to a local emergency department with 3 months of 30-lb weight loss associated with new painless jaundice. Evaluation revealed a 1.9 cm pancreatic head mass for which he underwent endoscopic ultrasound (EUS) with fine needle aspiration (FNA) and was discharged with hepatobiliary surgery follow-up. Prior to FNA results returning, he again presented to the emergency room, this time with altered mental status. Labs revealed a fingerstick glucose > 501 mg/dL, beta-hydroxybutyrate of 7.6 mmol/L, an anion gap of 17 with a venous blood gas showing pH 7.28 and bicarbonate 18 mEq/L, consistent with DKA. Other notable labs included ALT 126 U/L, bilirubin (total 5.7; direct 3.7 mg/dL), alkaline phosphatase 2,269 U/L, CA 19-9 of 2,699 U/mL, low C-peptide (0.3 ng/ml), and Hemoglobin A1c of 13.7%. He was treated with an insulin drip and intravenous fluids until resolution of DKA and return to baseline mental status. After surgical resection of the mass, the definitive diagnosis was stage IIB invasive PDAC. His initial requirement of 18 units of insulin glargine decreased to 4 units post-operatively.
Discussion: Multiple studies have now demonstrated hyperglycemia and weight loss in the months prior to PDAC diagnosis. Only a few case reports have linked PDAC, an exocrine pancreatic cancer, with DKA, a presentation more classically associated with endocrine pancreatic tumors. In our case, we identified a low C-peptide level suggesting low endogenous insulin production and pancreatic beta cell dysfunction, less commonly seen in patients with T2DM. We hypothesized this likely indicated a new-onset inability of the pancreas to produce insulin possibly due to local tumor invasion or a paraneoplastic phenomenon. Recent literature favors a paraneoplastic effect as the trigger of new-onset diabetes in PDAC given improvement in glycemic control after tumor resection, also observed in our case study. Further studies are needed to delineate the mechanism of beta cell dysfunction in PDAC.
Disclosures:
Marlon J. Brewer, MD, Edward Cytryn, MD, Valerie Moscoso, MD, Eric Barna, MD, Aimee L. Lucas, MD, MS. P1840 - Diabetic Ketoacidosis as Early Presentation of Pancreatic Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Pancreatic Ductal Adenocarcinoma (PDAC) is the 3rd leading cause of cancer related death in the United States. The bidirectional relationship between PDAC and diabetes is under study to determine if changes in metabolic parameters can predict cancer development. While new-onset diabetes is a well-described early manifestation of PDAC, we report a rare case of diabetic ketoacidosis (DKA) as the early presentation of PDAC.
Case Description/Methods: A 68-year-old man with chronic non-insulin dependent type 2 diabetes (T2DM) presented to a local emergency department with 3 months of 30-lb weight loss associated with new painless jaundice. Evaluation revealed a 1.9 cm pancreatic head mass for which he underwent endoscopic ultrasound (EUS) with fine needle aspiration (FNA) and was discharged with hepatobiliary surgery follow-up. Prior to FNA results returning, he again presented to the emergency room, this time with altered mental status. Labs revealed a fingerstick glucose > 501 mg/dL, beta-hydroxybutyrate of 7.6 mmol/L, an anion gap of 17 with a venous blood gas showing pH 7.28 and bicarbonate 18 mEq/L, consistent with DKA. Other notable labs included ALT 126 U/L, bilirubin (total 5.7; direct 3.7 mg/dL), alkaline phosphatase 2,269 U/L, CA 19-9 of 2,699 U/mL, low C-peptide (0.3 ng/ml), and Hemoglobin A1c of 13.7%. He was treated with an insulin drip and intravenous fluids until resolution of DKA and return to baseline mental status. After surgical resection of the mass, the definitive diagnosis was stage IIB invasive PDAC. His initial requirement of 18 units of insulin glargine decreased to 4 units post-operatively.
Discussion: Multiple studies have now demonstrated hyperglycemia and weight loss in the months prior to PDAC diagnosis. Only a few case reports have linked PDAC, an exocrine pancreatic cancer, with DKA, a presentation more classically associated with endocrine pancreatic tumors. In our case, we identified a low C-peptide level suggesting low endogenous insulin production and pancreatic beta cell dysfunction, less commonly seen in patients with T2DM. We hypothesized this likely indicated a new-onset inability of the pancreas to produce insulin possibly due to local tumor invasion or a paraneoplastic phenomenon. Recent literature favors a paraneoplastic effect as the trigger of new-onset diabetes in PDAC given improvement in glycemic control after tumor resection, also observed in our case study. Further studies are needed to delineate the mechanism of beta cell dysfunction in PDAC.
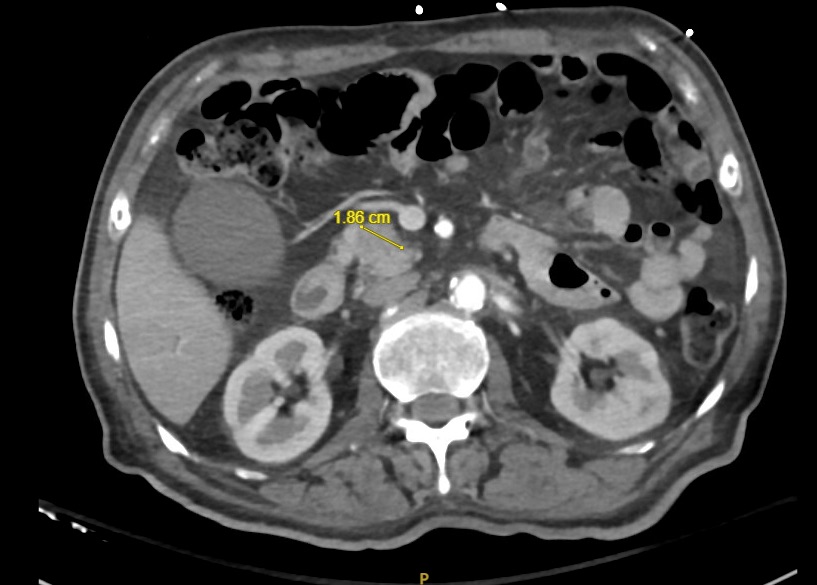
Figure: CT with 1.9 cm Pancreatic Head Mass
Disclosures:
Marlon Brewer indicated no relevant financial relationships.
Edward Cytryn indicated no relevant financial relationships.
Valerie Moscoso indicated no relevant financial relationships.
Eric Barna indicated no relevant financial relationships.
Aimee Lucas indicated no relevant financial relationships.
Marlon J. Brewer, MD, Edward Cytryn, MD, Valerie Moscoso, MD, Eric Barna, MD, Aimee L. Lucas, MD, MS. P1840 - Diabetic Ketoacidosis as Early Presentation of Pancreatic Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
