Monday Poster Session
Category: Biliary/Pancreas
P1842 - IPMN Diagnosis Made by Investigating Rapid Worsening of Glycemic Control in a Patient With Type II DM
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Hussam Almasri, MD, MRCP
University of North Dakota
Fargo, ND
Presenting Author(s)
Hussam Almasri, MD, MRCP1, James Fowler, MD2, Guneet Sidhu, MD1, Hallie Thompson, MD2, John Bassett, MD, FACG3
1University of North Dakota, Fargo, ND; 2University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 3Sanford Health, Fargo, ND
Introduction: Intraductal papillary mucinous neoplasms (IPMNs) of the pancreas are considered precancerous lesions especially the ones involving the main pancreatic duct (PD). These mucinous epithelial lesions can have various degrees of dysplasia. The management can range from surveillance to resection depending on the character of the lesion (cystic vs solid component), dysplasia, and size. IPMNs can be associated with pancreatic insufficiency but rarely isolated endocrine deficiencies. We present a patient who has type II diabetes mellitus (DM) with progressively worsening glycemic control and was found to have IPMN on screening imaging.
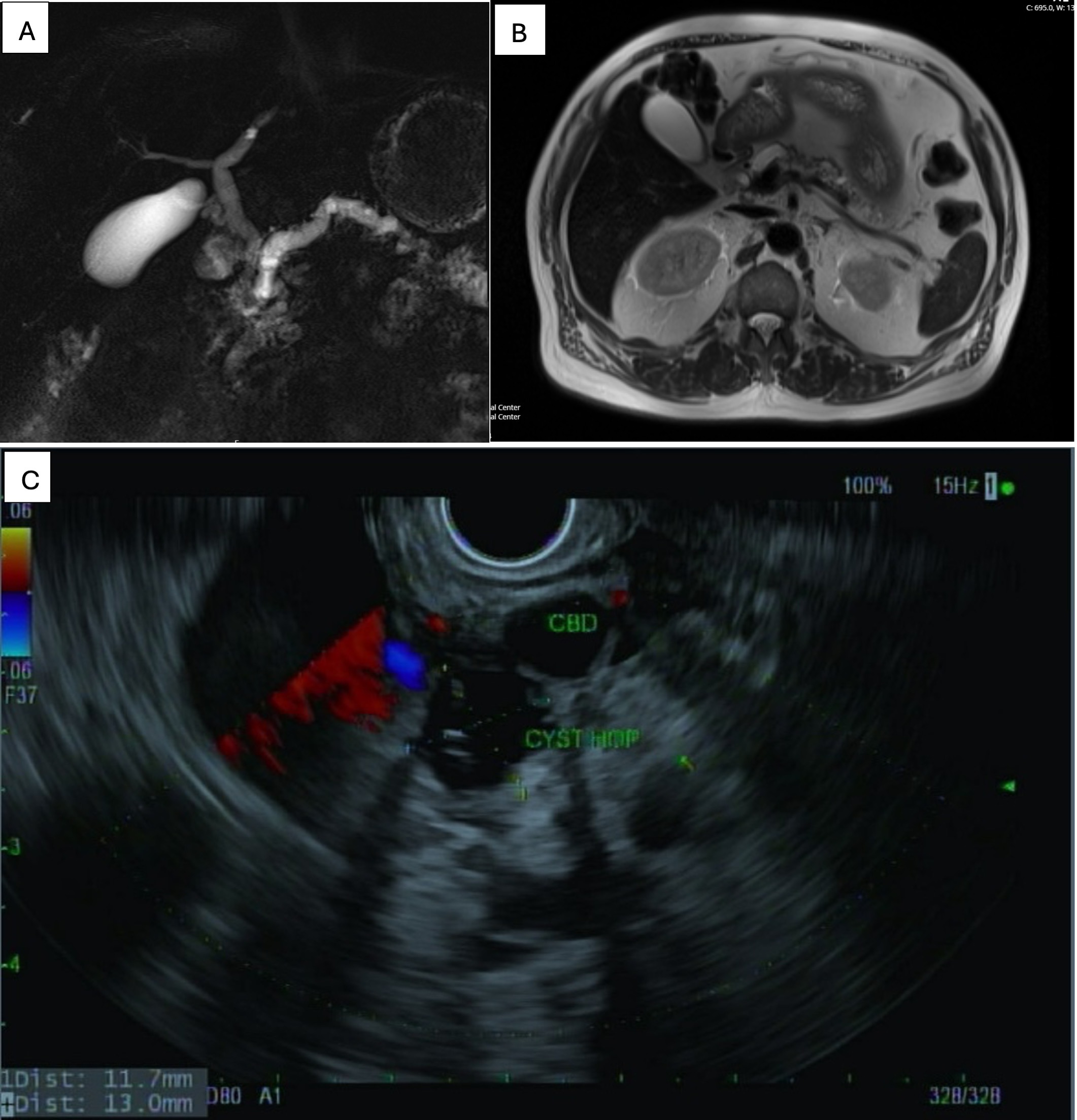
Case Description/Methods: A 64-year-old man with a known medical history of HTN and type II DM on lifestyle modifications. No significant alcohol use. Upon routine follow-up in the primary care clinic, HbA1c was done and found to be > 14 increasing from 6.8 one year before. Glucose in the clinic was 400 mg/dl. The patient did not have new symptoms, abdominal pain, weight changes, no new medications. Physical examination was unremarkable except for a BMI of 32 kg/m2. Other blood tests including CBC, renal, and liver functions were within normal limits. Acute complications were ruled out and the patient was started on insulin. A CT scan of the abdomen with contrast was done to rule out pancreatic pathology in the settings of progressive DM showed dilatation of the main PD confirmed by MRI. No pancreatic masses were identified. EUS/ERCP was consistent with the main duct IPMN with PD stricture and biliary dilatation (Figure. 1). A Plastic stent was placed in the PD and another one in the common bile duct. Histopathology from cytology/FNA/pancreatic duct biopsies were all consistent with mucinous epithelium with low-grade dysplasia. CA19-9 was negative. The patient was then referred for surgical oncology and opted for surveillance. After starting on insulin, DM has been well controlled.
Discussion: Management of IPMN is important to prevent or detect progression to pancreatic cancer which usually carries a poor prognosis at the time of diagnosis. New onset DM especially in older individuals is an important marker for pancreatic cancer. However, the association between new-onset DM or worsening glycemic control in diabetic patients and IPMN is less studied. It seems that worsening glycemic control can predict more PD or whole-gland IPMN rather than branch IPMN. Further research is required to establish guidelines on when to screen for pancreatic IPMN/Cancer in patients with DM.
Disclosures:
Hussam Almasri, MD, MRCP1, James Fowler, MD2, Guneet Sidhu, MD1, Hallie Thompson, MD2, John Bassett, MD, FACG3. P1842 - IPMN Diagnosis Made by Investigating Rapid Worsening of Glycemic Control in a Patient With Type II DM, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Dakota, Fargo, ND; 2University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 3Sanford Health, Fargo, ND
Introduction: Intraductal papillary mucinous neoplasms (IPMNs) of the pancreas are considered precancerous lesions especially the ones involving the main pancreatic duct (PD). These mucinous epithelial lesions can have various degrees of dysplasia. The management can range from surveillance to resection depending on the character of the lesion (cystic vs solid component), dysplasia, and size. IPMNs can be associated with pancreatic insufficiency but rarely isolated endocrine deficiencies. We present a patient who has type II diabetes mellitus (DM) with progressively worsening glycemic control and was found to have IPMN on screening imaging.
Case Description/Methods: A 64-year-old man with a known medical history of HTN and type II DM on lifestyle modifications. No significant alcohol use. Upon routine follow-up in the primary care clinic, HbA1c was done and found to be > 14 increasing from 6.8 one year before. Glucose in the clinic was 400 mg/dl. The patient did not have new symptoms, abdominal pain, weight changes, no new medications. Physical examination was unremarkable except for a BMI of 32 kg/m2. Other blood tests including CBC, renal, and liver functions were within normal limits. Acute complications were ruled out and the patient was started on insulin. A CT scan of the abdomen with contrast was done to rule out pancreatic pathology in the settings of progressive DM showed dilatation of the main PD confirmed by MRI. No pancreatic masses were identified. EUS/ERCP was consistent with the main duct IPMN with PD stricture and biliary dilatation (Figure. 1). A Plastic stent was placed in the PD and another one in the common bile duct. Histopathology from cytology/FNA/pancreatic duct biopsies were all consistent with mucinous epithelium with low-grade dysplasia. CA19-9 was negative. The patient was then referred for surgical oncology and opted for surveillance. After starting on insulin, DM has been well controlled.
Discussion: Management of IPMN is important to prevent or detect progression to pancreatic cancer which usually carries a poor prognosis at the time of diagnosis. New onset DM especially in older individuals is an important marker for pancreatic cancer. However, the association between new-onset DM or worsening glycemic control in diabetic patients and IPMN is less studied. It seems that worsening glycemic control can predict more PD or whole-gland IPMN rather than branch IPMN. Further research is required to establish guidelines on when to screen for pancreatic IPMN/Cancer in patients with DM.
Figure: Figure 1 A an MRCP reconstruction image showing the gallbladder and dilated PD. B MRI abdomen image showing IPMN. C EUS image showing cystic lesion with thickened wall 18 by 17 mm in maximum diameter.
Disclosures:
Hussam Almasri indicated no relevant financial relationships.
James Fowler indicated no relevant financial relationships.
Guneet Sidhu indicated no relevant financial relationships.
Hallie Thompson indicated no relevant financial relationships.
John Bassett indicated no relevant financial relationships.
Hussam Almasri, MD, MRCP1, James Fowler, MD2, Guneet Sidhu, MD1, Hallie Thompson, MD2, John Bassett, MD, FACG3. P1842 - IPMN Diagnosis Made by Investigating Rapid Worsening of Glycemic Control in a Patient With Type II DM, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
