Monday Poster Session
Category: Biliary/Pancreas
P1847 - A Rare Case of Pancreatitis Following Esophagogastroduodenoscopy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Benna Jacob, DO
NYU Langone Health
Mineola, NY
Presenting Author(s)
Benna Jacob, DO, Vincent Wong, MD, Umair Nasir, DO, Bhawna Halwan, MD
NYU Langone Health, Mineola, NY
Introduction: Acute pancreatitis can carry mortality as high as 30%. It is commonly caused by alcohol use and choledocholithiasis but can be associated with hypertriglyceridemia, hypercalcemia, medications, trauma, and endoscopic retrograde cholangiopancreatography. Here, we report a rare case of acute pancreatitis after a recent esophagogastroduodenoscopy (EGD).
Case Description/Methods: 86-year-old female with a history of coronary artery disease, atrial fibrillation, hypertension, and hyperlipidemia presented with symptomatic iron deficiency anemia and melena for two weeks. She denies any nausea, vomiting, abdominal pain, constipation, diarrhea, hematochezia, or NSAID use but does take apixaban and clopidogrel.
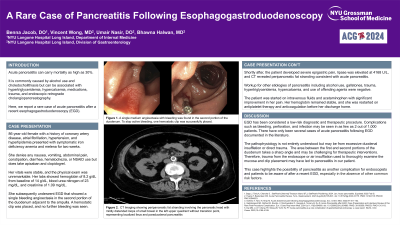
Her vitals were stable, and the physical exam was unremarkable. Her labs showed hemoglobin of 8.2 g/dL from baseline of 14 g/dL, blood urea nitrogen of 23 mg/dL, and creatinine of 1.09 mg/dL. She subsequently underwent EGD that showed a single bleeding angioectasia in the second portion of the duodenum adjacent to the ampulla. A hemostatic clip was placed, and no further bleeding was seen. Shortly after, the patient developed severe epigastric pain, lipase was elevated at 4168 U/L, and CT revealed peripancreatic fat stranding consistent with acute pancreatitis.
Workup for other etiologies of pancreatitis including alcohol use, gallstones, trauma, hypertriglyceridemia, hypercalcemia, and use of offending agents were negative. The patient was started on intravenous fluids and acetaminophen with significant improvement in her pain. Her hemoglobin remained stable, and she was restarted on antiplatelet therapy and anticoagulation before her discharge home.
Discussion: EGD has been considered a low-risk diagnostic and therapeutic procedure. Complications such as bleeding, perforation, and infection may be seen in as few as 2 out of 1,000 patients. There have only been several cases of acute pancreatitis following EGD documented in the literature. The pathophysiology is not entirely understood but may be from excessive duodenal insufflation or direct trauma. The area between the first and second portions of the duodenum takes a sharp angle and may be challenging for therapeutic interventions. Therefore, trauma from the endoscope, air insufflation used to thoroughly examine the mucosa or placement of the clip may have led to pancreatitis in our patient. This case highlights the possibility of pancreatitis as another complication for endoscopists and patients to be aware of after a recent EGD.
Disclosures:
Benna Jacob, DO, Vincent Wong, MD, Umair Nasir, DO, Bhawna Halwan, MD. P1847 - A Rare Case of Pancreatitis Following Esophagogastroduodenoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
NYU Langone Health, Mineola, NY
Introduction: Acute pancreatitis can carry mortality as high as 30%. It is commonly caused by alcohol use and choledocholithiasis but can be associated with hypertriglyceridemia, hypercalcemia, medications, trauma, and endoscopic retrograde cholangiopancreatography. Here, we report a rare case of acute pancreatitis after a recent esophagogastroduodenoscopy (EGD).
Case Description/Methods: 86-year-old female with a history of coronary artery disease, atrial fibrillation, hypertension, and hyperlipidemia presented with symptomatic iron deficiency anemia and melena for two weeks. She denies any nausea, vomiting, abdominal pain, constipation, diarrhea, hematochezia, or NSAID use but does take apixaban and clopidogrel.
Her vitals were stable, and the physical exam was unremarkable. Her labs showed hemoglobin of 8.2 g/dL from baseline of 14 g/dL, blood urea nitrogen of 23 mg/dL, and creatinine of 1.09 mg/dL. She subsequently underwent EGD that showed a single bleeding angioectasia in the second portion of the duodenum adjacent to the ampulla. A hemostatic clip was placed, and no further bleeding was seen. Shortly after, the patient developed severe epigastric pain, lipase was elevated at 4168 U/L, and CT revealed peripancreatic fat stranding consistent with acute pancreatitis.
Workup for other etiologies of pancreatitis including alcohol use, gallstones, trauma, hypertriglyceridemia, hypercalcemia, and use of offending agents were negative. The patient was started on intravenous fluids and acetaminophen with significant improvement in her pain. Her hemoglobin remained stable, and she was restarted on antiplatelet therapy and anticoagulation before her discharge home.
Discussion: EGD has been considered a low-risk diagnostic and therapeutic procedure. Complications such as bleeding, perforation, and infection may be seen in as few as 2 out of 1,000 patients. There have only been several cases of acute pancreatitis following EGD documented in the literature. The pathophysiology is not entirely understood but may be from excessive duodenal insufflation or direct trauma. The area between the first and second portions of the duodenum takes a sharp angle and may be challenging for therapeutic interventions. Therefore, trauma from the endoscope, air insufflation used to thoroughly examine the mucosa or placement of the clip may have led to pancreatitis in our patient. This case highlights the possibility of pancreatitis as another complication for endoscopists and patients to be aware of after a recent EGD.
Disclosures:
Benna Jacob indicated no relevant financial relationships.
Vincent Wong indicated no relevant financial relationships.
Umair Nasir indicated no relevant financial relationships.
Bhawna Halwan indicated no relevant financial relationships.
Benna Jacob, DO, Vincent Wong, MD, Umair Nasir, DO, Bhawna Halwan, MD. P1847 - A Rare Case of Pancreatitis Following Esophagogastroduodenoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
