Monday Poster Session
Category: Biliary/Pancreas
P1848 - Endoscopic Cystogastrostomy for Management of Large Pancreatic Pseudocyst
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Gurjot Singh, DO
The Warren Alpert Medical School of Brown University
Warwick, RI
Presenting Author(s)
Gurjot Singh, DO1, Seetha Lakshmanan, MD2, Kailtyn M. Egger, DO2
1The Warren Alpert Medical School of Brown University, Warwick, RI; 2Kent Hospital, Warwick, RI
Introduction: Pancreatic cystogastrostomy is a technique that creates a conduit between a pancreatic pseudocyst and the stomach allowing for drainage of large fluid collections. Here we present a patient requiring endoscopic placement of a cystogastrostomy stent secondary to a large pancreatic pseudocyst.
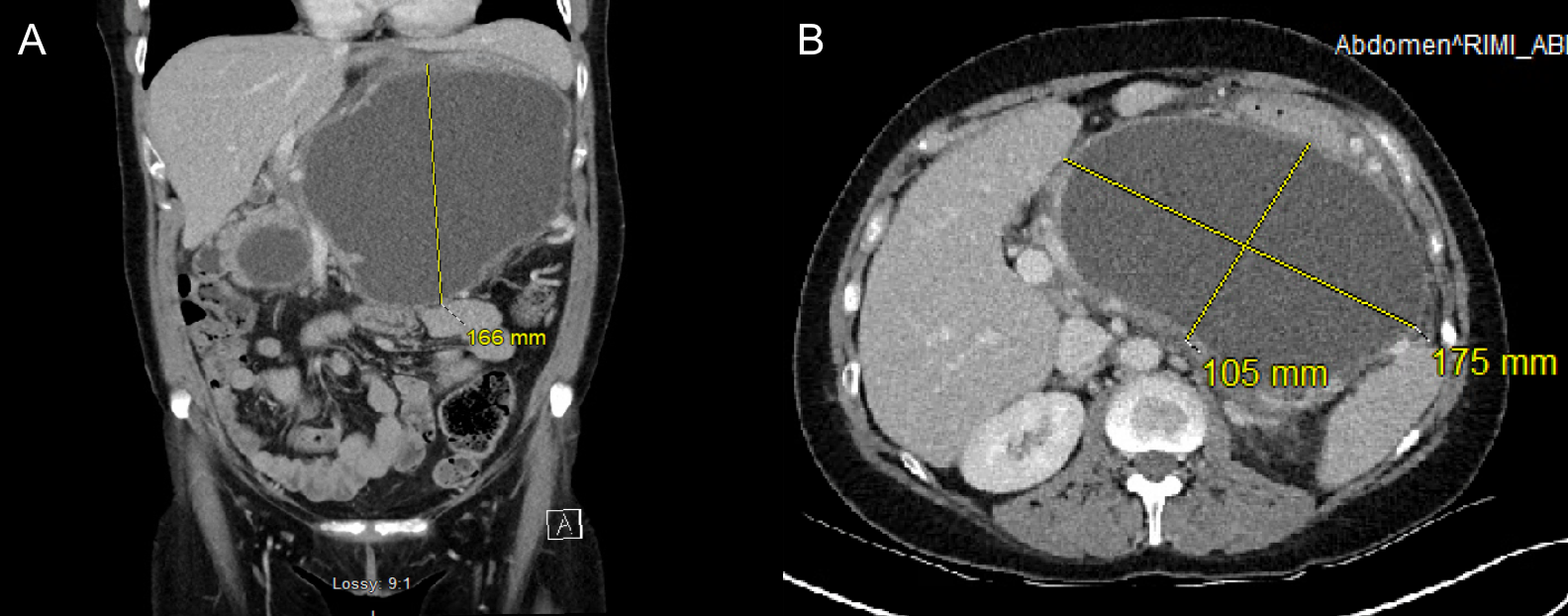
Case Description/Methods: A 37-year-old female with alcohol use disorder presented to the emergency room with complaints of epigastric pain. Physical exam was notable for distended abdomen. Labs demonstrated an elevated WBC of 20.8x10^3/mcL, normal LFTs, normal lipase, and elevated ethanol level. CT abdomen and pelvis with contrast showed a 10.5 x 17.5 x 16.6 cm pancreatic pseudocyst within the pancreatic body. Also noted was a delayed left nephrogram secondary to extrinsic compression on the left adrenal vein. She then underwent EUS which revealed an anechoic, 12 x 8cm lesion filled with fluid and debris in the pancreatic body. Doppler imaging was used to identify interposed vessels that were normal. A 2.0 x 1.0cm Axios stent was then deployed between the pancreatic body and gastric wall, and dilated to 1.5 cm. Her clinical course was complicated by acute pancreatitis 2 weeks post-stent placement. Repeat CT abdomen then demonstrated a new fluid collection in the pancreatic head measuring 6.3 x 5.1 cm with overall resolution of initial pancreatic pseudocyst. The patient was managed conservatively and EUS was repeated 3 weeks later which showed the unchanged size of the pancreatic head pseudocyst with no intervention. The previous Axios stent was removed with rat tooth forceps. The patient was clinically stable during follow-up.
Discussion: Small pancreatic pseudocysts are usually monitored conservatively whereas symptomatic patients with persistently large or complicated pancreatic pseudocysts due to hemorrhage or infection often require intervention. Endoscopic cystogastrostomy may offer benefits to patients who are poor surgical candidates and have large pancreatic pseudocysts to the extent where anatomical structures may undergo extrinsic compression, such as the left adrenal vein in this case. Overall, endoscopic cystogastrostomy is preferred to surgical intervention due to its continuous drainage, minimally invasive approach, and decreased patient-dependent management of external drains.
Disclosures:
Gurjot Singh, DO1, Seetha Lakshmanan, MD2, Kailtyn M. Egger, DO2. P1848 - Endoscopic Cystogastrostomy for Management of Large Pancreatic Pseudocyst, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Warren Alpert Medical School of Brown University, Warwick, RI; 2Kent Hospital, Warwick, RI
Introduction: Pancreatic cystogastrostomy is a technique that creates a conduit between a pancreatic pseudocyst and the stomach allowing for drainage of large fluid collections. Here we present a patient requiring endoscopic placement of a cystogastrostomy stent secondary to a large pancreatic pseudocyst.
Case Description/Methods: A 37-year-old female with alcohol use disorder presented to the emergency room with complaints of epigastric pain. Physical exam was notable for distended abdomen. Labs demonstrated an elevated WBC of 20.8x10^3/mcL, normal LFTs, normal lipase, and elevated ethanol level. CT abdomen and pelvis with contrast showed a 10.5 x 17.5 x 16.6 cm pancreatic pseudocyst within the pancreatic body. Also noted was a delayed left nephrogram secondary to extrinsic compression on the left adrenal vein. She then underwent EUS which revealed an anechoic, 12 x 8cm lesion filled with fluid and debris in the pancreatic body. Doppler imaging was used to identify interposed vessels that were normal. A 2.0 x 1.0cm Axios stent was then deployed between the pancreatic body and gastric wall, and dilated to 1.5 cm. Her clinical course was complicated by acute pancreatitis 2 weeks post-stent placement. Repeat CT abdomen then demonstrated a new fluid collection in the pancreatic head measuring 6.3 x 5.1 cm with overall resolution of initial pancreatic pseudocyst. The patient was managed conservatively and EUS was repeated 3 weeks later which showed the unchanged size of the pancreatic head pseudocyst with no intervention. The previous Axios stent was removed with rat tooth forceps. The patient was clinically stable during follow-up.
Discussion: Small pancreatic pseudocysts are usually monitored conservatively whereas symptomatic patients with persistently large or complicated pancreatic pseudocysts due to hemorrhage or infection often require intervention. Endoscopic cystogastrostomy may offer benefits to patients who are poor surgical candidates and have large pancreatic pseudocysts to the extent where anatomical structures may undergo extrinsic compression, such as the left adrenal vein in this case. Overall, endoscopic cystogastrostomy is preferred to surgical intervention due to its continuous drainage, minimally invasive approach, and decreased patient-dependent management of external drains.
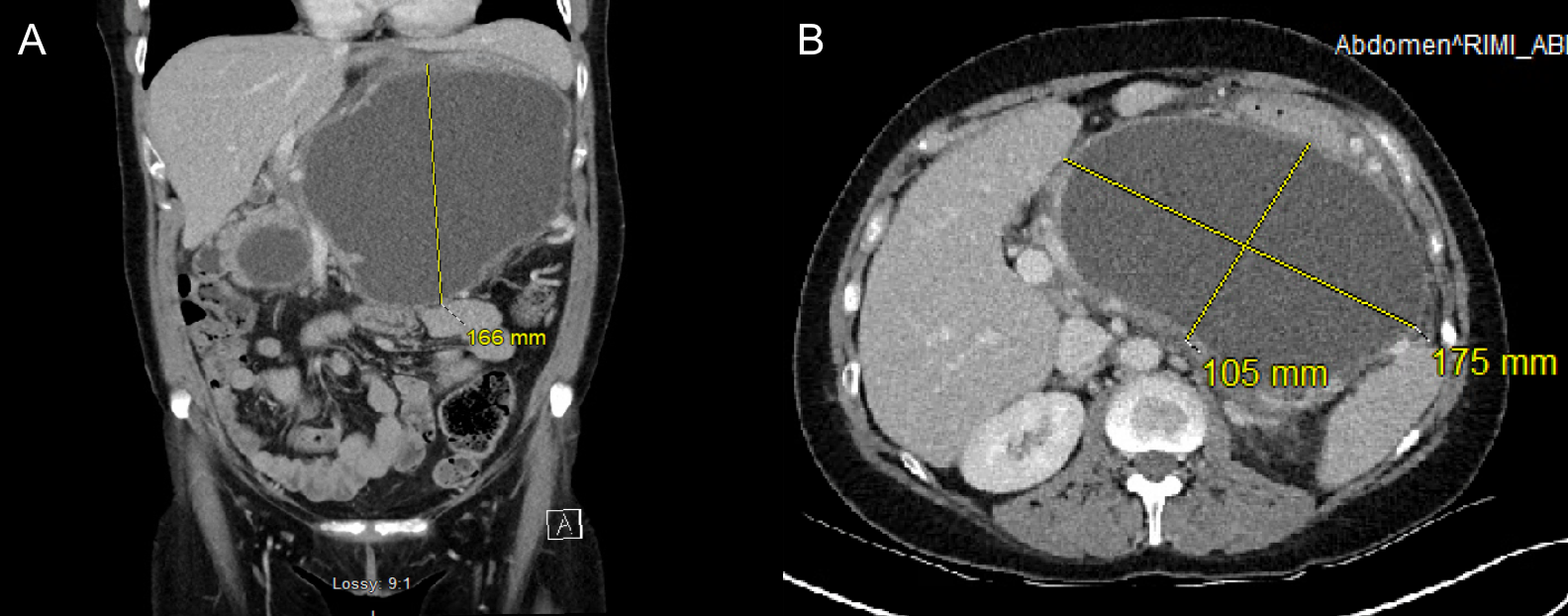
Figure: Computed tomography of the abdomen and pelvis with contrast A.) Axial view of pseudocyst collection spanning a height of 16.6cm. B.) Coronal view of pseudocyst collection with a length and width of17.5cm and 10.5cm, respectively.
Disclosures:
Gurjot Singh indicated no relevant financial relationships.
Seetha Lakshmanan indicated no relevant financial relationships.
Kailtyn Egger indicated no relevant financial relationships.
Gurjot Singh, DO1, Seetha Lakshmanan, MD2, Kailtyn M. Egger, DO2. P1848 - Endoscopic Cystogastrostomy for Management of Large Pancreatic Pseudocyst, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
