Monday Poster Session
Category: Biliary/Pancreas
P1858 - Using a Self-Migrating Pancreatic Stent for Treatment of Papillitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Moshe Spira, MD
Westchester Medical Center
Fair Lawn, NJ
Presenting Author(s)
Moshe Spira, MD, Zilan Lin, MD, Wei Tang, MD, Virendra Tewari, MD, FACG
Westchester Medical Center, Valhalla, NY
Introduction: Papillitis of the major duodenal papilla is a rare phenomenon that can lead to abdominal pain and biliary obstruction. The limited available data, mostly consisting of case reports, have discussed the significance of clinical scenarios and subsequent management. Typically, endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy, with or without biliary stenting, is needed to relieve biliary obstruction caused by papillitis. To our knowledge, this is the first reported case of papillitis resulting in biliary obstruction that occurred after biliary stent removal and was successfully treated with a single pigtail, self-migrating pancreatic stent, without the need for a repeat procedure for stent removal.
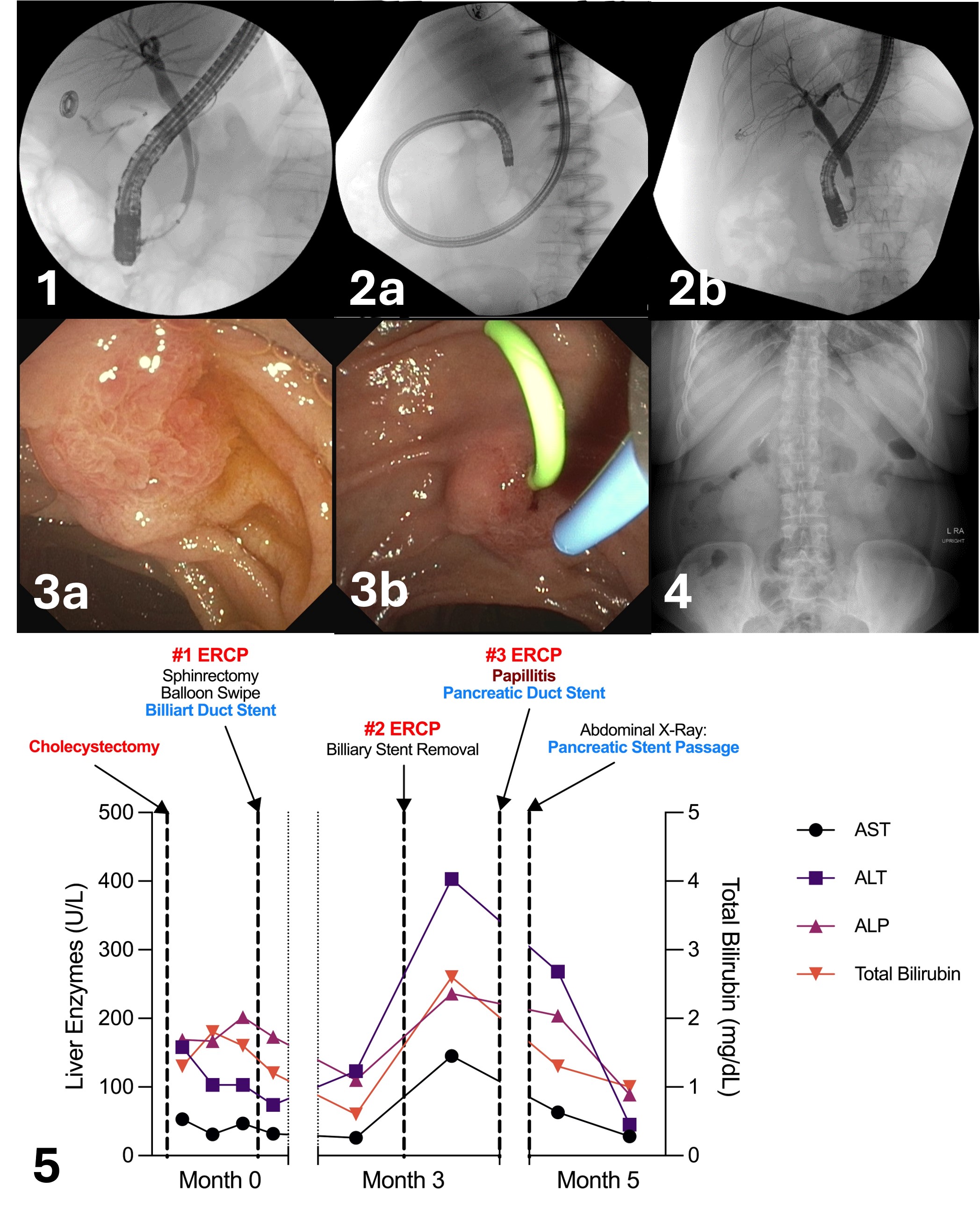
Case Description/Methods: A 57-year-old female presented to the emergency department (ED) with worsening right upper quadrant abdominal pain a week after cholecystectomy. Liver function tests (LFTs) were elevated, and cross-sectional imaging was positive for a bile leak. The patient underwent ERCP, which demonstrated a leak from the cystic duct stump. Sphincterotomy and balloon swipes were performed, and a 7 cm by 19 French straight biliary stent was placed. LFTs subsequently normalized. The biliary stent was removed three months later during a repeat ambulatory ERCP when no contrast leak was noted. However, two days after the procedure, the patient presented to the ED with scleral icterus and elevated LFTs again. A third ERCP was performed and revealed an erythematous major papilla and mild biliary dilatation without residual stone or sludge, raising suspicion of papillitis. To avoid the need for another ERCP, a 5 cm by 5 French Advanix™ single pigtail pancreatic stent was placed in the common bile duct to relieve the biliary obstruction. LFTs started to improve the next day. The patient followed up at the outpatient office 2.5 weeks later, and an X-ray confirmed the passage of the stent. LFTs were also normalized and another ERCP was avoided. Figure 3 illustrates the timeline of the patient’s disease course and interventions.
Discussion: Our case demonstrated the feasibility of managing papillitis of the major duodenal papilla using a self-migrating pancreatic stent, mitigating the need for an additional ERCP for stent removal.
Disclosures:
Moshe Spira, MD, Zilan Lin, MD, Wei Tang, MD, Virendra Tewari, MD, FACG. P1858 - Using a Self-Migrating Pancreatic Stent for Treatment of Papillitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Westchester Medical Center, Valhalla, NY
Introduction: Papillitis of the major duodenal papilla is a rare phenomenon that can lead to abdominal pain and biliary obstruction. The limited available data, mostly consisting of case reports, have discussed the significance of clinical scenarios and subsequent management. Typically, endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy, with or without biliary stenting, is needed to relieve biliary obstruction caused by papillitis. To our knowledge, this is the first reported case of papillitis resulting in biliary obstruction that occurred after biliary stent removal and was successfully treated with a single pigtail, self-migrating pancreatic stent, without the need for a repeat procedure for stent removal.
Case Description/Methods: A 57-year-old female presented to the emergency department (ED) with worsening right upper quadrant abdominal pain a week after cholecystectomy. Liver function tests (LFTs) were elevated, and cross-sectional imaging was positive for a bile leak. The patient underwent ERCP, which demonstrated a leak from the cystic duct stump. Sphincterotomy and balloon swipes were performed, and a 7 cm by 19 French straight biliary stent was placed. LFTs subsequently normalized. The biliary stent was removed three months later during a repeat ambulatory ERCP when no contrast leak was noted. However, two days after the procedure, the patient presented to the ED with scleral icterus and elevated LFTs again. A third ERCP was performed and revealed an erythematous major papilla and mild biliary dilatation without residual stone or sludge, raising suspicion of papillitis. To avoid the need for another ERCP, a 5 cm by 5 French Advanix™ single pigtail pancreatic stent was placed in the common bile duct to relieve the biliary obstruction. LFTs started to improve the next day. The patient followed up at the outpatient office 2.5 weeks later, and an X-ray confirmed the passage of the stent. LFTs were also normalized and another ERCP was avoided. Figure 3 illustrates the timeline of the patient’s disease course and interventions.
Discussion: Our case demonstrated the feasibility of managing papillitis of the major duodenal papilla using a self-migrating pancreatic stent, mitigating the need for an additional ERCP for stent removal.
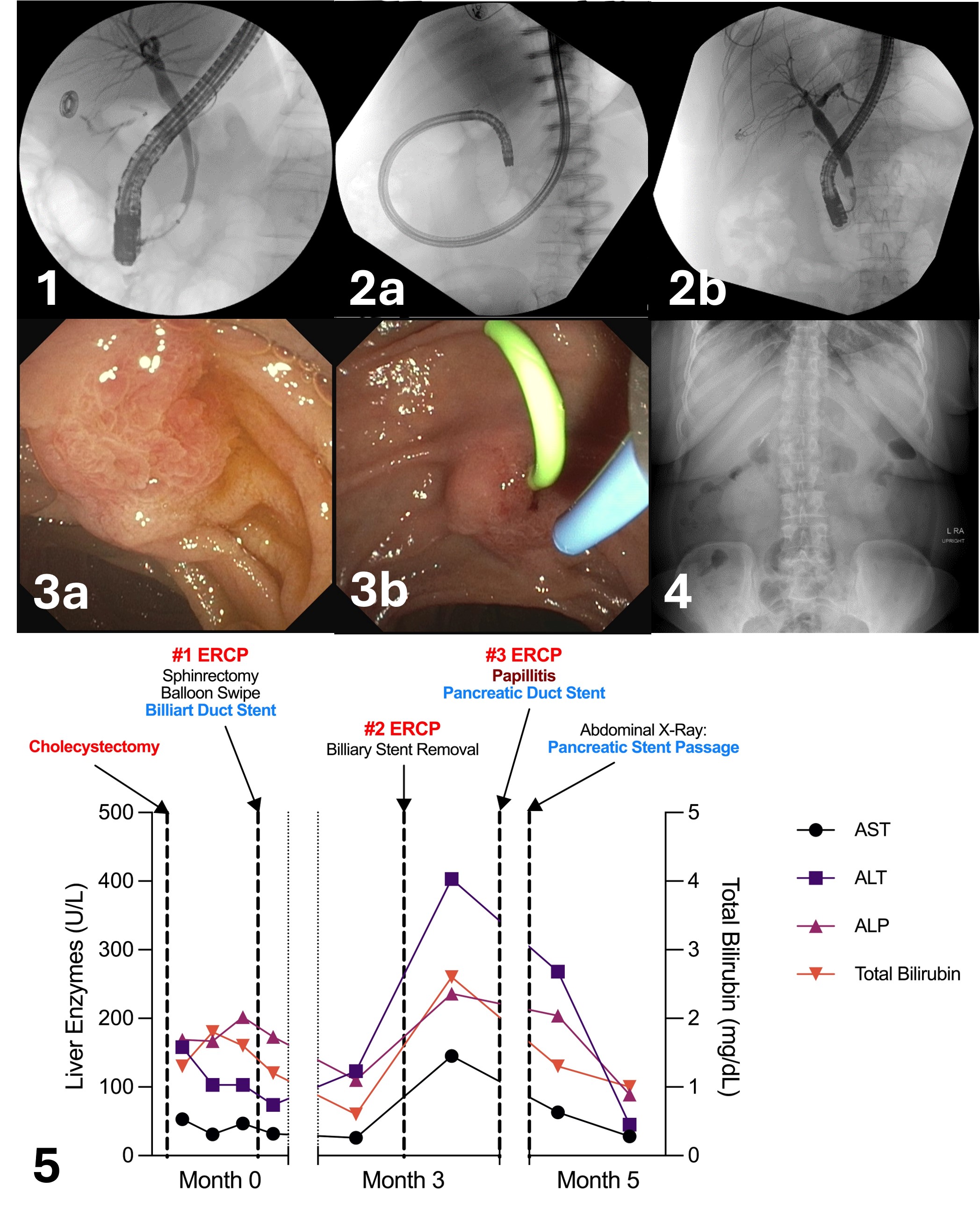
Figure: 1. Cholangiogram with biliary leak. 2a. Cholangiogram after biliary stent. 2b. Cholangiogram with resolution of biliary leak. 3a. ERCP with ampulla prior to ballooning and stenting. 3b. ERCP with pancreatic stent placement at ampulla. 4. Abdominal x-ray confirming passage of the pancreatic stent. 5. Timeline of LFTs/ALP/Total bilirubin changes with clinical events/ERCP interventions.
Disclosures:
Moshe Spira indicated no relevant financial relationships.
Zilan Lin indicated no relevant financial relationships.
Wei Tang indicated no relevant financial relationships.
Virendra Tewari indicated no relevant financial relationships.
Moshe Spira, MD, Zilan Lin, MD, Wei Tang, MD, Virendra Tewari, MD, FACG. P1858 - Using a Self-Migrating Pancreatic Stent for Treatment of Papillitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
