Monday Poster Session
Category: Biliary/Pancreas
P1860 - An Unusual Presentation of Necrotizing Pancreatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Tessa Herman, MD
University of Minnesota and Minneapolis VA Health Care System
Minneapolis, MN
Presenting Author(s)
Tessa Herman, MD1, Rahul Karna, MD2, Petr Vanek, MD2, Nabeel Azeem, MD3, Guru Trikudanathan, MD2
1University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3University of Minnesota Medical Center, Minneapolis, MN
Introduction: Necrotizing pancreatitis can lead to fistulization, most commonly affecting the duodenum or colon. We present a case about a patient presenting with hematochezia later found to have necrotizing pancreatitis with a spontaneous cyst-colonic fistula.
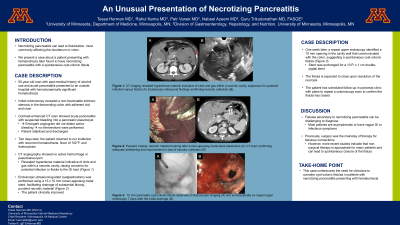
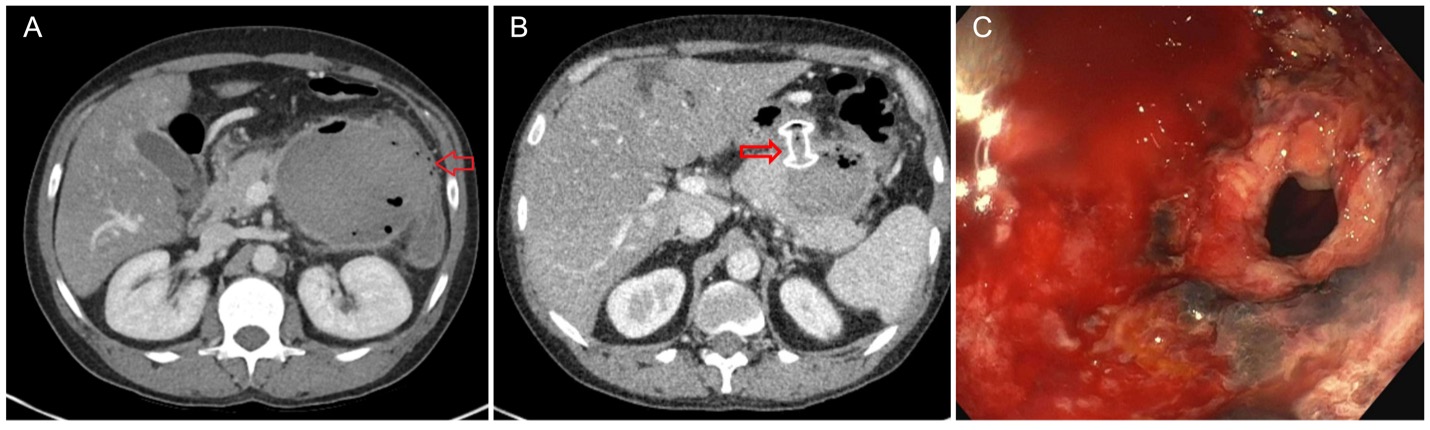
Case Description/Methods: A 50-year-old man with history of alcohol use and acute pancreatitis presented with hemodynamically significant hematochezia. Initial colonoscopy at an outside hospital revealed a non-traversable extrinsic stenosis in the descending colon with adherent clot and ulcer. Computerized tomography (CT) showed acute pancreatitis with suspected bleeding into a pancreatic pseudocyst, but emergent angiogram did not detect active bleeding. No interventions were performed. The patient stabilized and was discharged. He returned two days later with recurrent hematochezia, fevers of 102°F and leukocytosis. CT angiography showed no active hemorrhage or pseudoaneurysm, but it revealed hyperdense material indicative of clots and gas within a necrotic cavity, raising concerns for potential infection or a fistula to the gastrointestinal tract (Figure 1A). Endoscopic ultrasound-guided cystgastrostomy was performed using a 15 mm × 10 mm lumen-apposing metal stent, facilitating drainage of substantial bloody, purulent necrotic material (Figure 1B). The patient improved clinically after the procedure. Seven days later, a repeat upper endoscopy identified a 10mm opening in the cavity wall communicating with the colon, suggesting a spontaneous cyst-colonic fistula (Figure 1C). The stent was exchanged for a 10 Fr × 1 cm double-pigtail stent, and the fistula is expected to close upon resolution of the necrosis. The patient has scheduled follow-up in pancreas clinic with plans to repeat a colonoscopy soon to confirm the fistula has closed.
Discussion: Fistulas secondary to necrotizing pancreatitis can be challenging to diagnose given most patients are asymptomatic, or otherwise may present with vague gastrointestinal or infectious symptoms. While surgery used to be the mainstay of therapy, more recent studies have indicated that non-surgical therapy is appropriate for many patients resulting in spontaneous closure of the fistula. This case underscores the need for clinicians to consider cyst-colonic fistulas in patients with necrotizing pancreatitis presenting with hematochezia.
Disclosures:
Tessa Herman, MD1, Rahul Karna, MD2, Petr Vanek, MD2, Nabeel Azeem, MD3, Guru Trikudanathan, MD2. P1860 - An Unusual Presentation of Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3University of Minnesota Medical Center, Minneapolis, MN
Introduction: Necrotizing pancreatitis can lead to fistulization, most commonly affecting the duodenum or colon. We present a case about a patient presenting with hematochezia later found to have necrotizing pancreatitis with a spontaneous cyst-colonic fistula.
Case Description/Methods: A 50-year-old man with history of alcohol use and acute pancreatitis presented with hemodynamically significant hematochezia. Initial colonoscopy at an outside hospital revealed a non-traversable extrinsic stenosis in the descending colon with adherent clot and ulcer. Computerized tomography (CT) showed acute pancreatitis with suspected bleeding into a pancreatic pseudocyst, but emergent angiogram did not detect active bleeding. No interventions were performed. The patient stabilized and was discharged. He returned two days later with recurrent hematochezia, fevers of 102°F and leukocytosis. CT angiography showed no active hemorrhage or pseudoaneurysm, but it revealed hyperdense material indicative of clots and gas within a necrotic cavity, raising concerns for potential infection or a fistula to the gastrointestinal tract (Figure 1A). Endoscopic ultrasound-guided cystgastrostomy was performed using a 15 mm × 10 mm lumen-apposing metal stent, facilitating drainage of substantial bloody, purulent necrotic material (Figure 1B). The patient improved clinically after the procedure. Seven days later, a repeat upper endoscopy identified a 10mm opening in the cavity wall communicating with the colon, suggesting a spontaneous cyst-colonic fistula (Figure 1C). The stent was exchanged for a 10 Fr × 1 cm double-pigtail stent, and the fistula is expected to close upon resolution of the necrosis. The patient has scheduled follow-up in pancreas clinic with plans to repeat a colonoscopy soon to confirm the fistula has closed.
Discussion: Fistulas secondary to necrotizing pancreatitis can be challenging to diagnose given most patients are asymptomatic, or otherwise may present with vague gastrointestinal or infectious symptoms. While surgery used to be the mainstay of therapy, more recent studies have indicated that non-surgical therapy is appropriate for many patients resulting in spontaneous closure of the fistula. This case underscores the need for clinicians to consider cyst-colonic fistulas in patients with necrotizing pancreatitis presenting with hematochezia.
Figure: Figure 1 – Necrotizing Pancreatitis Complicated by Cyst-Colonic Fistula: Computer tomography (CT) imaging revealed hyperdense material indicative of clots and gas within a necrotic cavity, suspicious for potential infection versus fistula (Figure 1A), which was treated with endoscopic drainage with cystgastrostomy using a 15x10mm lumen apposing metal stent (Figure 1B). Repeat endoscopy for necrosectomy identified a 10mm opening in the cavity wall communicating with the colon, suggesting a spontaneous cyst-colonic fistula (Figure 1C).
Disclosures:
Tessa Herman indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Petr Vanek indicated no relevant financial relationships.
Nabeel Azeem: Boston Scientific – Consultant.
Guru Trikudanathan: AbbVie – Grant/Research Support. Boston Scientific – Consultant.
Tessa Herman, MD1, Rahul Karna, MD2, Petr Vanek, MD2, Nabeel Azeem, MD3, Guru Trikudanathan, MD2. P1860 - An Unusual Presentation of Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
