Monday Poster Session
Category: Biliary/Pancreas
P1886 - When Blood Meets Bile: A Novel Case of Cholangitis Due to Haemobilia
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Migara Jayasekera, MD
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Migara Jayasekera, MD, Muhammad Mushtaq, DO, Robinder Abrol, DO, Juliana Yang, MD
University of Texas Medical Branch, Galveston, TX
Introduction: Haemobilia, blood extravasation into the biliary tract, is a rare case of gastrointestinal bleeding (GIB). Common causes of haemobilia are iatrogenic, trauma, and neoplastic processes. The incidence is rising with the increase in minimally invasive pancreaticobiliary procedures. Presentation of haemobilia after liver trauma is rare, ~ 0.2%, but its presentation with biliary obstruction is extremely rare. Here, we present the first documented case of haemobilia-induced cholangitis due to liver trauma.
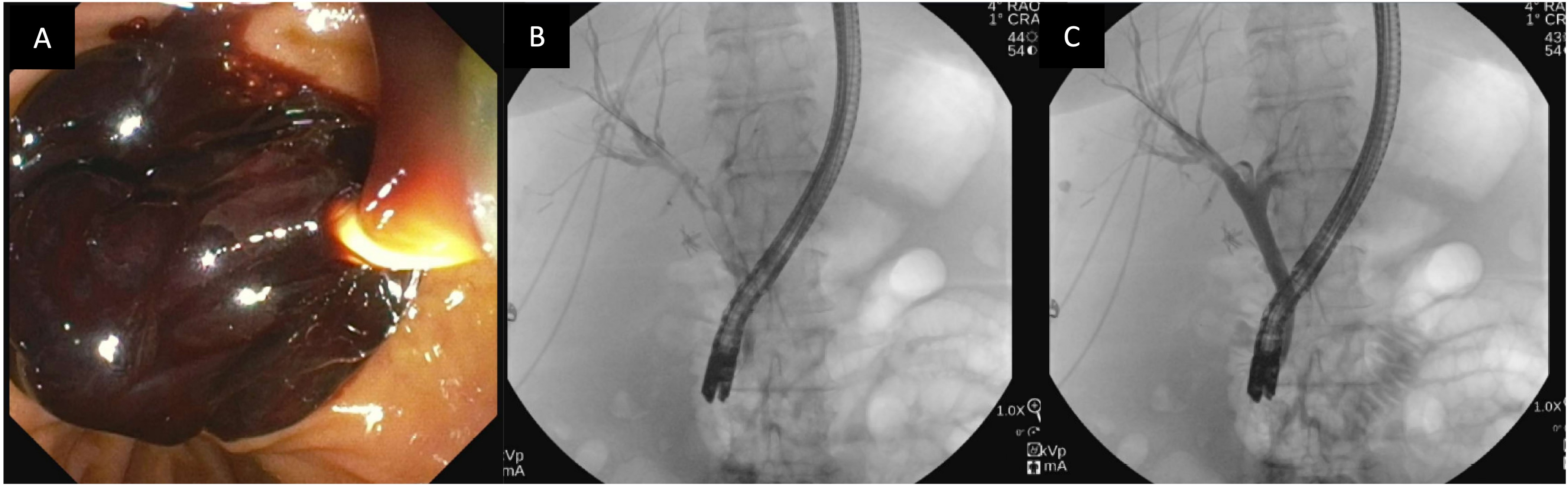
Case Description/Methods: A 72-year-old female with a past medical history of hypertension presented with nausea, vomiting, and severe right-sided rib pain after a ground-level fall. Labs were significant AST- 750, ALT-463, and Alk Phos- 96, which were attributed to alcohol use. The patient was discharged with a plan for supportive treatment. Given worsening pain and jaundice, the patient was re-evaluated in the ED. Subsequent labs were significant for total bilirubin-11.1 (conjugated bilirubin 8.1), Hgb-8.7 (reduced from 11.2), AST-353, ALT-506, and Alk Phos-740. CT abdomen showed a right hepatic lobe intraparenchymal hematoma with capsular tear and nondisplaced rib fractures. Subsequent HIDA scan showed two intrahepatic bilomas without bile leakage into the peritoneal cavity. She developed a fever and leukocytosis. Given concern for cholangitis, ERCP was done and showed a filling defect extending the entire length of the common bile duct due to a large intraductal clot for which biliary sphincterotomy with stenting of CBD was performed. The patient improved clinically with a reduction in bilirubin and leukocytosis. The patient later underwent right hepatic artery embolization and right perihepatic hematoma drain placement.
Discussion: Haemobilia classically presents with Quink’s Triad (Jaundice, right upper quadrant pain, and UGIB) found in 22-35% of cases. Rarely, it can present as cholangitis. While diagnosis is challenging, laboratory findings of anemia, hyperbilirubinemia, elevated aminotransaminase, and alkaline phosphatase levels can be suggestive of haemobilia. CT angiography is the first-line imaging modality for haemobilia diagnosis in unstable patients; however, given high sensitivity, US or MRI may precede CT. Resuscitation with catheter angiography is the standard of treatment, especially in unstable patients. Once hemostasis is achieved, endoscopic intervention is important for relieving the obstruction, which in some cases may proceed with catheter angiography, as in our case.
Disclosures:
Migara Jayasekera, MD, Muhammad Mushtaq, DO, Robinder Abrol, DO, Juliana Yang, MD. P1886 - When Blood Meets Bile: A Novel Case of Cholangitis Due to Haemobilia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas Medical Branch, Galveston, TX
Introduction: Haemobilia, blood extravasation into the biliary tract, is a rare case of gastrointestinal bleeding (GIB). Common causes of haemobilia are iatrogenic, trauma, and neoplastic processes. The incidence is rising with the increase in minimally invasive pancreaticobiliary procedures. Presentation of haemobilia after liver trauma is rare, ~ 0.2%, but its presentation with biliary obstruction is extremely rare. Here, we present the first documented case of haemobilia-induced cholangitis due to liver trauma.
Case Description/Methods: A 72-year-old female with a past medical history of hypertension presented with nausea, vomiting, and severe right-sided rib pain after a ground-level fall. Labs were significant AST- 750, ALT-463, and Alk Phos- 96, which were attributed to alcohol use. The patient was discharged with a plan for supportive treatment. Given worsening pain and jaundice, the patient was re-evaluated in the ED. Subsequent labs were significant for total bilirubin-11.1 (conjugated bilirubin 8.1), Hgb-8.7 (reduced from 11.2), AST-353, ALT-506, and Alk Phos-740. CT abdomen showed a right hepatic lobe intraparenchymal hematoma with capsular tear and nondisplaced rib fractures. Subsequent HIDA scan showed two intrahepatic bilomas without bile leakage into the peritoneal cavity. She developed a fever and leukocytosis. Given concern for cholangitis, ERCP was done and showed a filling defect extending the entire length of the common bile duct due to a large intraductal clot for which biliary sphincterotomy with stenting of CBD was performed. The patient improved clinically with a reduction in bilirubin and leukocytosis. The patient later underwent right hepatic artery embolization and right perihepatic hematoma drain placement.
Discussion: Haemobilia classically presents with Quink’s Triad (Jaundice, right upper quadrant pain, and UGIB) found in 22-35% of cases. Rarely, it can present as cholangitis. While diagnosis is challenging, laboratory findings of anemia, hyperbilirubinemia, elevated aminotransaminase, and alkaline phosphatase levels can be suggestive of haemobilia. CT angiography is the first-line imaging modality for haemobilia diagnosis in unstable patients; however, given high sensitivity, US or MRI may precede CT. Resuscitation with catheter angiography is the standard of treatment, especially in unstable patients. Once hemostasis is achieved, endoscopic intervention is important for relieving the obstruction, which in some cases may proceed with catheter angiography, as in our case.
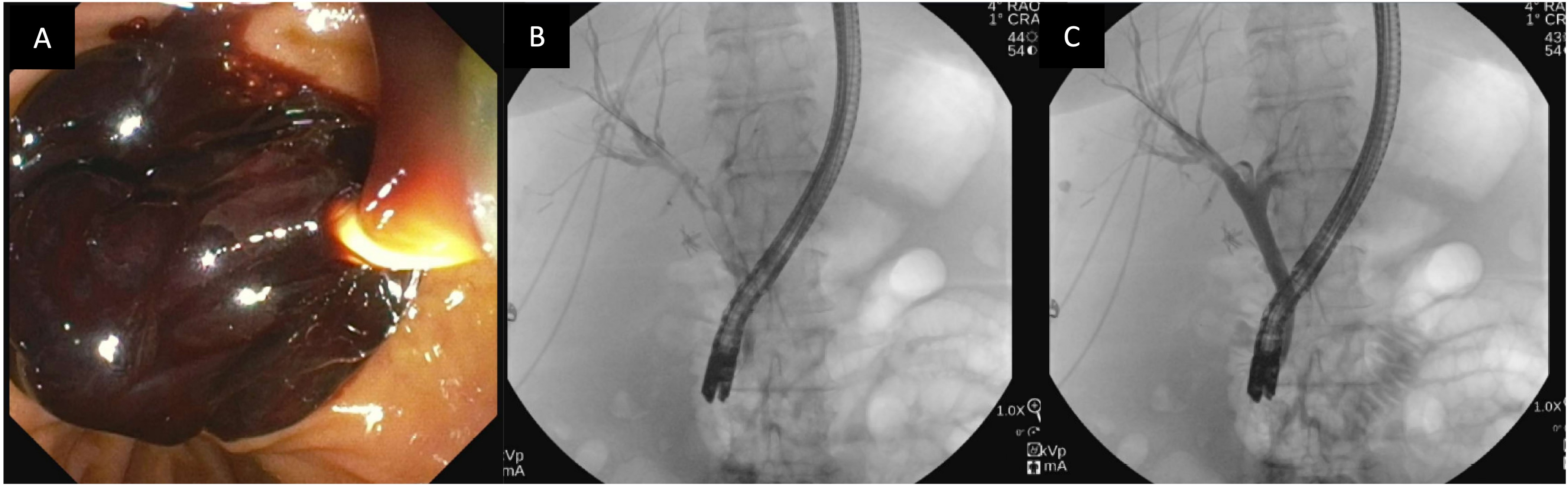
Figure: A- Intraductal clot during sphincterotomy with sweeping of the biliary tree. B- Pre-sphincterotomy Cholangiogram showing a filling defect along the entire common bile duct. C- Post-sphincterotomy cholangiogram demonstrating patency throughout the biliary tree.
Disclosures:
Migara Jayasekera indicated no relevant financial relationships.
Muhammad Mushtaq indicated no relevant financial relationships.
Robinder Abrol indicated no relevant financial relationships.
Juliana Yang indicated no relevant financial relationships.
Migara Jayasekera, MD, Muhammad Mushtaq, DO, Robinder Abrol, DO, Juliana Yang, MD. P1886 - When Blood Meets Bile: A Novel Case of Cholangitis Due to Haemobilia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
